With cancer treatments drastically transforming in the last decade, radionuclide drug conjugates (RDCs) offer effective, precise treatment and diagnosis while minimizing side effects. RDCs worldwide have already received regulatory approval, and more will soon follow as researchers aim to continue improving efficacy, safety, and personalization. In this article, we dive into RDCs’ benefits and challenges.
What are RDCs?
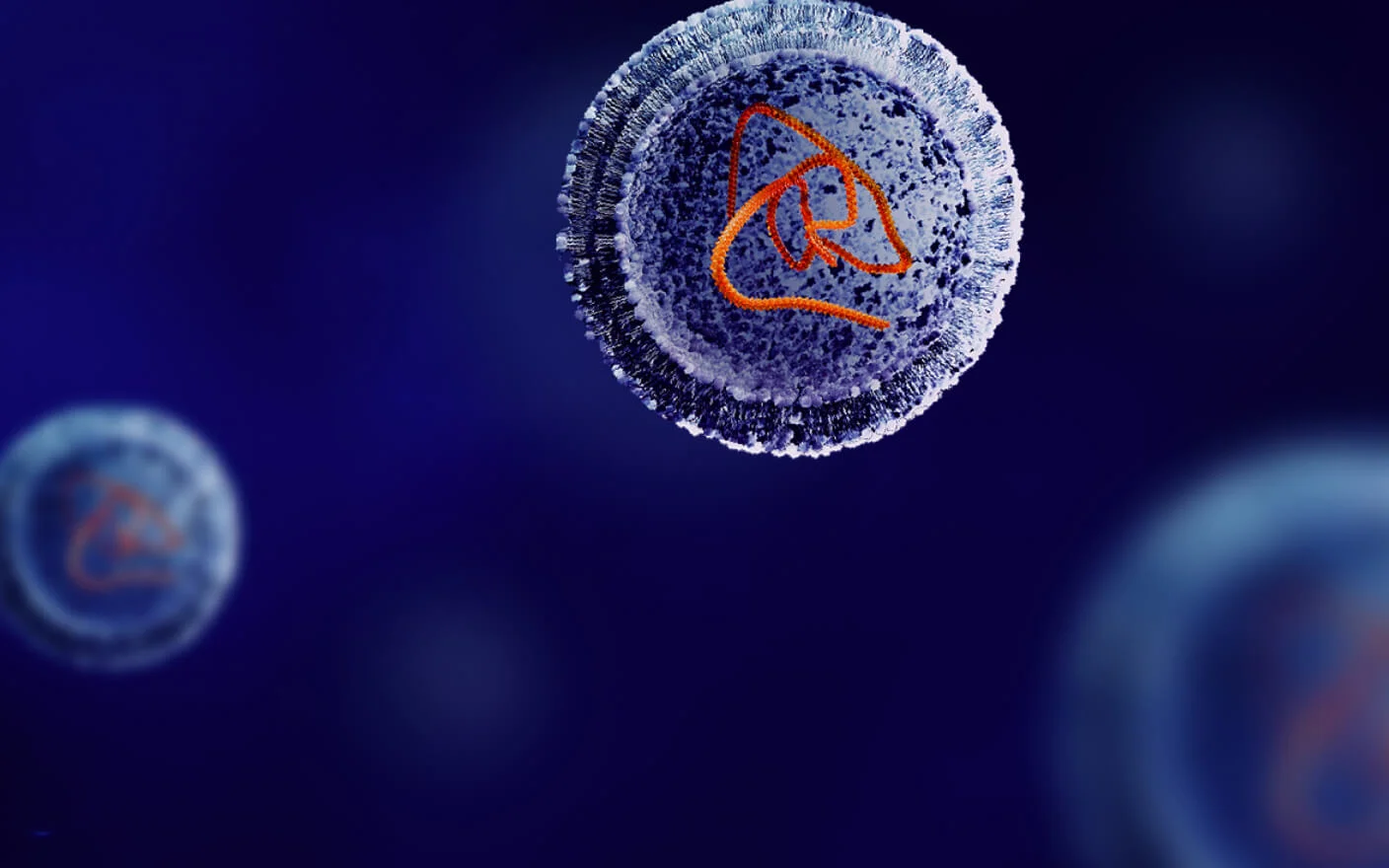
Traditional cancer treatment uses radiotherapy, delivering radiation from outside of the body. The problem with this approach is the inability to differentiate between normal cells and cancerous tumor cells. This causes significant off-target toxicity and jeopardizes patient health. RDCs attack only the cancerous cells, delivering radiation more effectively and targeting tumors in a way that greatly reduces side effects.
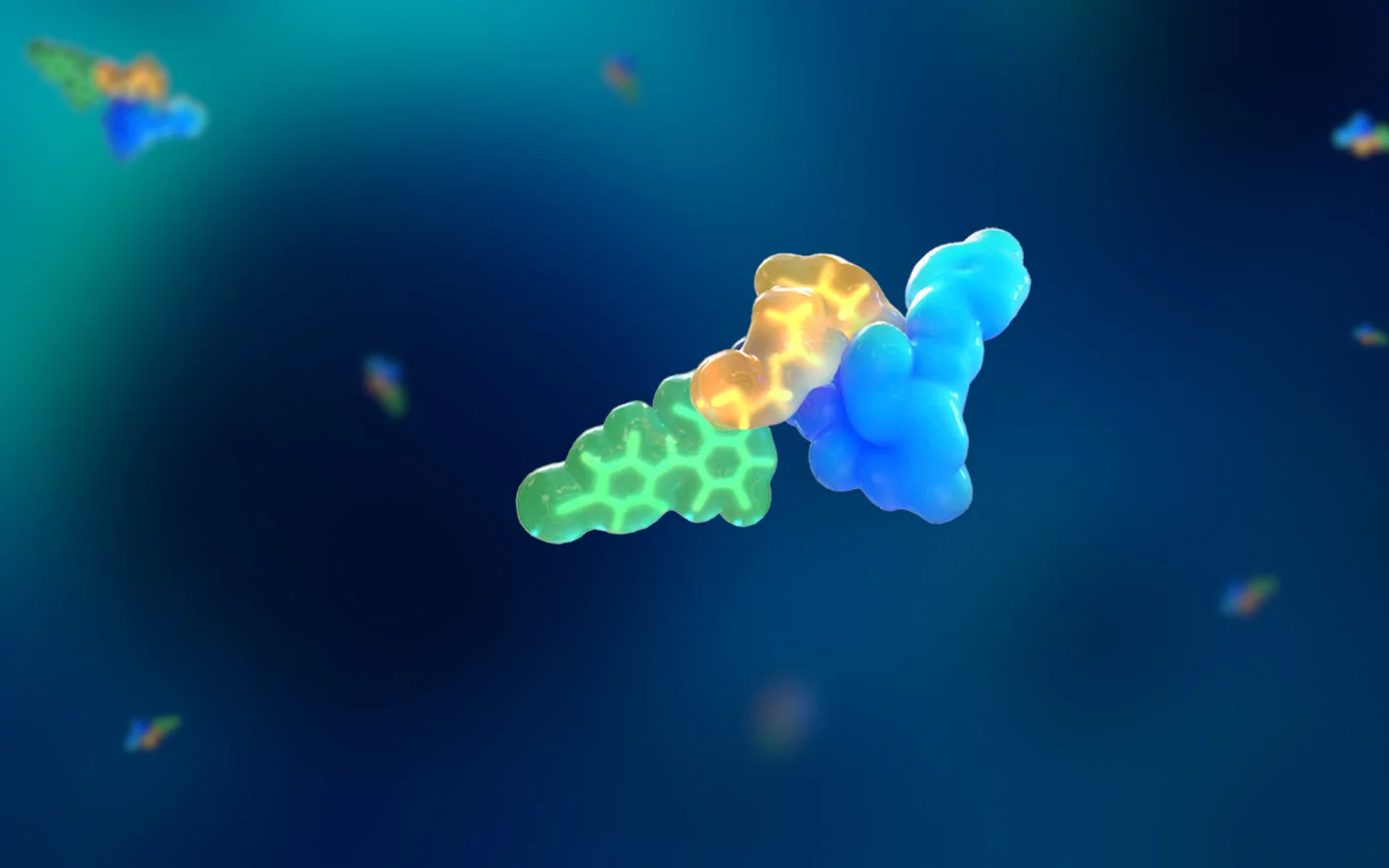
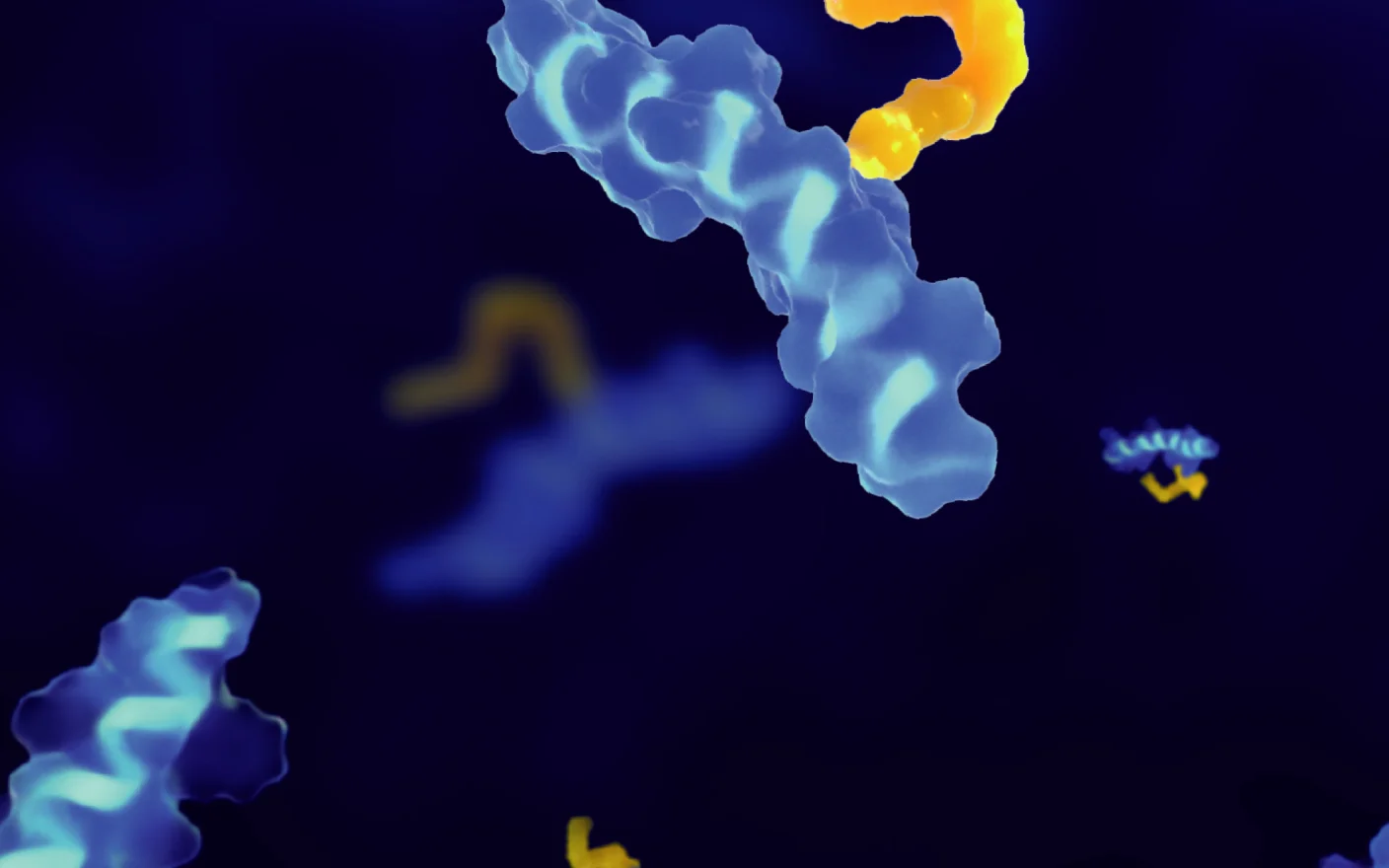
RDCs are made up of four components:
The radionuclide, a radioactive atom that emits radiation, is capable of killing a cancerous cell. It can emit particles or rays and release energy to diagnose and provide therapy to a patient.
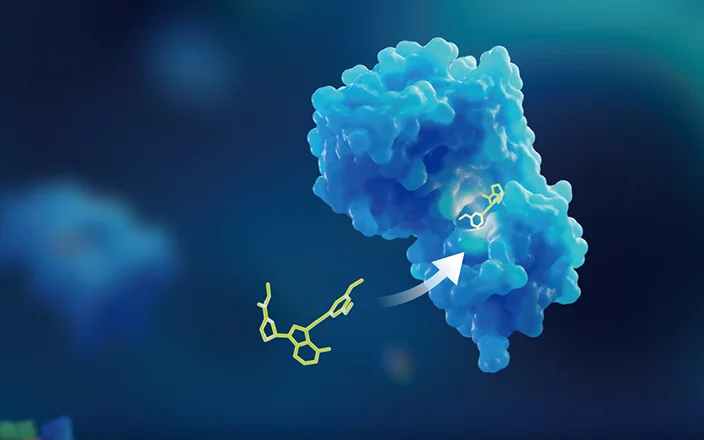
The targeting molecule acts like a homing beacon, locating and binding to disease cells. The targeting molecule can be a peptide, antibody, or other substance that has a high affinity to a receptor or antigen on a disease cell.
The chelator binds the radionuclide, ensuring it is securely in place and can be delivered to the diseased cells without affecting healthy tissue.
The linker plays a critical role in the safety and stability of the RDC. It connects the targeting molecule to the chelator and binds it to the radionuclide.
The evolution of RDCs
In the early 20th century, radium-226 was one of the first radionuclides used in the treatment of various diseases, pioneering the field of radiotherapy. The use of iodine-131 for cancer treatment began in the 1940s, with significant advancements occurring in 1946. Iodine-131 proved effective in treating thyroid cancer and introduced a minimally invasive therapy for this condition. This breakthrough demonstrated to researchers that radionuclides could be effectively employed to target specific cancers. In the years following, Abbott Laboratories, among other companies, made substantial contributions to the development of radiopharmaceuticals, further advancing cancer treatment.
With rapid progress over the next several decades, nine RDCs have been approved by American regulators since 2016, including seven for cancer diagnoses and two for cancer therapy.
Advantages of RDCs
While other therapies can target similar diseases, RDCs offer several advantages, including:
Minimizing drug resistance: Traditional therapies, including small molecules and biologics, rely on signal pathways and targets, which makes them prone to drug resistance. Cancer cells are highly adaptable, able to mutate to find new pathways to continue their destructive growth. Conversely, RDCs rely on direct irradiation from radionuclides, which breaks down DNA and triggers the cancer cells to die.
Locating tumors: RDCs can quickly and reliably locate a tumor. Traditional methods of diagnosing tumors include CT, MRI, and biopsy. However, CT and MRI results can take a long time as various personnel must conduct and interpret the results—while patients are stuck waiting. Biopsies are invasive and, depending on their location, risky. Biopsy results can also rely heavily on the doctor’s skills at removal and interpretation. Some sites, such as bone metastasis, are impossible to sample, but RDCs can reach these sites and identify tumor metastasis through molecular images.
Integrating diagnostics and therapy: During diagnostic imaging, some radionuclides emit positrons or photons to measure the location of tumors. After the imaging is completed, RDCs equipped with α-, β- or Auger particle-emitting nuclides can be used for treatment. However, doctors can treat patients more effectively by integrating diagnosis and therapy. RDCs can provide more precise information about a tumor, including its size, location, and the specific antigens it expresses. This allows treatments to be tailored to the patient, enabling personalized medicine.
Challenges of RDC development
While RDCs have enormous potential, developing them can be challenging. The supply of radioactive nuclides is limited, and their use is subject to strict qualifications and environmental protections. Their short half-life also adds a logistics challenge, limiting the time they can be used, often hours or days. As a result, they must be produced and transported quickly from a nearby facility, with distribution tailored to the immediate needs of medical staff.
Because RDCs are novel, navigating regulatory requirements can be demanding. Regulatory bodies expect a wealth of data to fully understand the benefits and risks. Drug developers lacking the required in-house expertise should leverage a trusted and experienced lab partner to manage this environment effectively.
A final word
RDCs have made significant progress in a short timeframe, but there is still much to be done. Efforts are underway to combine the effects of RDCs with inhibitors of DNA repair factors to stop tumors from reversing the damage done by therapies. RDCs are also being combined with immune checkpoint inhibitors to improve patient outcomes. Researchers developing new RDCs face challenges as they bring therapies to market, but with efficient and safe testing, they can introduce new treatments in the fight against cancer.
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, and clinical drug metabolism and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,600+ global clients, and have successfully supported 1,500+ IND applications.
Talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Related Services and Platforms




Stay Connected
Keep up with the latest news and insights.