Drug metabolism refers to the process in which a drug undergoes structural changes under the action of various drug-metabolizing enzymes (primarily in the liver). It is also known as biotransformation and is one of the major focuses of pharmacokinetic research. Notably, the drugs are metabolized into non-pharmacologically active metabolites or pharmacologically active metabolites, or even toxic metabolites. The activity or safety concerns arising from these metabolites can significantly impact the success or failure of drug development to some extent.

Figure 1: General Pathway of Drug Metabolism.1
Despite over two decades of research on Proteolysis-Targeting Chimera (PROTAC)*, there are no PROTAC drugs that have been approved for the market and little literature on PROTAC metabolism. This article summarizes the studies on the metabolism of PROTAC molecules according to the literature and the practical experience of WuXi AppTec DMPK to assist researchers in studying PROTAC molecules. The main parts of this article are as follows: (1) understanding the key metabolic enzymes of PROTAC, (2) selecting an appropriate in vitro PROTAC metabolism model, and (3) facilitating structural optimization through studies on metabolic soft spots.
Understanding the key metabolic enzymes of PROTAC
Firstly, it is critical to identify the enzymes that may participate in PROTAC metabolism, the same with small molecule drugs. The molecular weight of PROTAC compounds is about 600-1200, which is slightly larger than that of conventional small molecules (the molecular weight of compounds meeting the Lipinski Rule is generally less than 500). Considering the PROTAC is a ternary complex that is composed of two small molecular compounds linked through linkers, its metabolism may be more complex. Common drug-metabolizing enzymes involved in small molecule metabolism mainly include phase I metabolizing enzymes (CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP3A etc.) and phase II metabolizing enzymes (UDP-glucuronosyltransferases (UGTs), sulfotransferases (SULTs), etc.). The enzyme system of phase I metabolism, represented by CYP450 enzymes, is considered to be involved in the metabolism of about 50% of clinical drugs.2

Figure 2: Drug Metabolism involved in CYP and Non-CYP.2
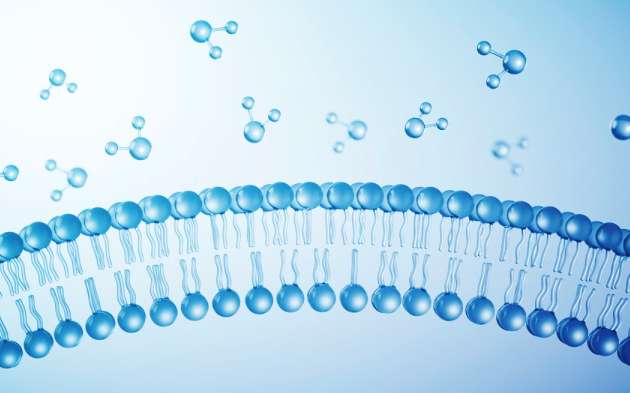
Goracci et al.3 reported that CYP3A4 and human aldehyde oxidase (hAOX) are involved in PROTAC metabolism. CYP3A4 is the most major phase I metabolizing enzyme among the CYP450 enzymes. However, as a cytosolic drug-metabolizing enzyme that is mainly expressed in the liver, aldehyde oxidase (AO) is a non-CYP drug-metabolizing enzyme. It is worth noting that there are marked species differences in the metabolism of AO, with large individual differences in rats, almost no expression in dogs, and the most expression in humans.4 Therefore, although compounds that are mainly metabolized by AO are metabolically stable in animals, they may be metabolically unstable in humans. As the metabolism of AO is neglected in early development, some candidate compounds are terminated due to rapid clearance and low bioavailability. From the perspective of drug screening, the metabolism of AO should be identified as early as possible.

Figure 3: Structure of Human Aldehyde Oxidase.5
Additionally, in vitro plasma or whole blood stability is another important metabolic system of PROTAC screening at an early stage. We found that PROTAC molecules have various degrees of whole blood stability problems according to the experimental data. The whole blood contains rich hydrolases that can catalyze the hydrolysis metabolism of drugs. Compounds with functional groups, such as ester bonds, amide bonds, sulfonamide bonds and peptide bonds may unstable in whole blood. Some PROTAC molecules in plasma or whole blood are unstable, which may be caused by the instability of linker or linker binding sites.
Overall, the drug-metabolizing enzymes involved in PROTAC metabolism are phase I or phase II metabolizing enzymes involved in the metabolism of conventional small molecules. For the types of metabolizing enzymes, attention needs to be paid to PROTAC metabolism by CYP3A4, aldehyde oxidase, and hydrolase in whole blood. Aldehyde oxidase, in particular, is not a common metabolizing enzyme. As shown in Figure 2, aldehyde oxidase and xanthine oxidase (XO) only involve in the metabolism of about 3% of the drugs on the market. In addition, further study on identifying particular enzymes that may cause the instability of PROTAC in whole blood needs to be conducted.
Selecting an appropriate in vitro PROTAC metabolism model
Some metabolic models, including liver microsomes, hepatocytes, and liver S9, are usually used in the in vitro metabolism of small molecules and are also applicable to PROTAC molecules. The appropriate in vitro metabolic model can be selected according to PROTAC metabolism characteristics. Studies found that the metabolic rates of some PROTAC compounds using liver microsomes or hepatocytes respectively may differ significantly. This has also been confirmed in our studies. Liver microsomes mainly contain phase I metabolizing enzymes and their metabolism can better reflect the in vitro metabolism when compounds are mainly metabolized by CYP enzymes. However, when there is strong non-phase I metabolism, the hepatocyte system is more appropriate. The mentioned aldehyde oxidase is a drug-metabolizing enzyme in the cytosol, and its content in liver microsomes is low. Hepatocyte contains a membrane barrier and complete metabolizing enzyme system so it is an appropriate system for studying the in vitro metabolism of PROTAC.

Figure 4: Study Model of PROTAC In Vitro Metabolism
It is necessary to study the metabolism of aldehyde oxidase specifically if aldehyde oxidase may be involved in PROTAC metabolism. As aldehyde oxidase exists in the cytosol, it can be studied via liver S9 or the liver cytosol system. At the same time, the effects on metabolism with or without aldehyde oxidase inhibitors need to be investigated. If aldehyde oxidase participates in metabolism, the metabolic rate with or without aldehyde oxidase inhibitors may be different.
There may be stability problems with PROTAC in whole blood or plasma. The most direct assessment method is to investigate the stability of PROTAC compounds in whole blood/plasma in vitro. The conventional incubation time (about 2 hours at most) could meet the needs of in vitro study of PROTAC molecules. Our study found that the stability data obtained from whole blood and plasma may be quite different. It is speculated that the enzyme activities of frozen plasma may be different from that of freshly collected whole blood. Therefore, it is recommended to use freshly collected whole blood to study metabolic stability.
It is worth noting that the protein binding rate of PROTAC molecules is generally high, and the free concentrations in the incubation system need to be fully considered when the interspecies comparison or in vitro-in vivo extrapolation (IVIVE) is conducted. It is recommended to conduct IVIVE after the protein binding rate has been accurately determined. It was reported that in vitro-in vivo correlation was good by using the in vitro hepatocyte data of mice, with the theoretical in vivo clearance of most PROTAC molecules within threefold of the actual value.6

Figure 5: Analysis of In Vitro-In Vivo Correlation of PROTAC Metabolism via Hepatocytes.6
Facilitating structural optimization through studies on PROTAC metabolic soft spots.
The PROTAC molecule is a ternary complex formed by connecting two ligands via a linker. Linker cleavage or metabolism of two ligands are possible metabolic sites. Goracci et al3 compared the metabolic soft spots and metabolic rates of the PROTAC molecule and its ligands, drawing the following conclusions:
1. The metabolic soft spot of PROTAC might be completely different from that of ligands.
2. The linker cleavage site of PROTAC is a common metabolic site.
3. The metabolic rate of PROTAC might be completely different from that of ligands.
Therefore, it was difficult to predict the metabolism of PROTAC molecules according to the metabolism of ligands. PROTAC metabolism shall be studied as a whole. Furthermore, the linker cleavage site is a metabolic type of PROTAC that is different from conventional small molecules.6 Linker cleavage can produce two ligand-related PROTAC metabolites, which may have the following characteristics:
1. The metabolic clearance rates are completely different from that of PROTAC;
2. The protein binding rates are lower than that of PROTAC due to the small molecular weight;
3. Two ligands are intact in their structure so that the target protein or E3 ligase can be bound.
If there are obvious Linker cleavage metabolites, the effect of metabolites on drug efficacy needs to be fully considered in the PK/PD study of PROTAC. In addition, possible safety problems associated with metabolites shall be studied as needed.

Figure 6: Linker Cleavage Metabolites Produced by PROTAC.6
Conclusion
PROTAC metabolism can be evaluated and predicted by various in vitro metabolic models. At present, it is difficult to identify which models are completely appropriate or inappropriate for PROTAC metabolism. It has been reported that good prediction results can be obtained by in vitro-in vivo extrapolation via hepatocyte metabolic data, but this does not mean that the method is suitable for all PROTAC molecules. During the screening process, it is recommended to summarize the metabolic characteristics of the same series of PROTAC compounds, selectively conduct metabolic studies, and find an in vitro metabolic model appropriate for PROTAC molecules to predict in vivo clearance or evaluate the early screening of compounds. In view of the study on PROTAC metabolism, we expect more experience to be summarized in order to gain an in-depth understanding of the metabolic characteristics of PROTAC molecules.
Click here to learn more about the strategies for PROTAC, or talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
*PROTAC® is a registered trademark of Arvinas. In this article, PROTAC specifically refers to the abbreviation of Proteolysis-Targeting Chimera as therapeutic modalities.
Authors: Liping Ma, Chengyuan Li, Jing Jin
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,500+ global clients, and have successfully supported 1,200+ IND applications.
Reference
1 Wang D, Liu W, Shen Z, Jiang L, Wang J, Li S, Li H. Deep Learning Based Drug Metabolites Prediction. Front Pharmacol. 2020 Jan 30;10:1586. doi: 10.3389/fphar.2019.01586. PMID: 32082146; PMCID: PMC7003989.
2 Saravanakumar A, Sadighi A, Ryu R, Akhlaghi F. Physicochemical Properties, Biotransformation, and Transport Pathways of Established and Newly Approved Medications: A Systematic Review of the Top 200 Most Prescribed Drugs vs. the FDA-Approved Drugs Between 2005 and 2016. Clin Pharmacokinet. 2019 Oct;58(10):1281-1294. doi: 10.1007/s40262-019-00750-8. PMID: 30972694; PMCID: PMC6773482.
3 Goracci L, Desantis J, Valeri A, Castellani B, Eleuteri M, Cruciani G. Understanding the Metabolism of Proteolysis Targeting Chimeras (PROTACs): The Next Step toward Pharmaceutical Applications. J Med Chem. 2020 Oct 22;63(20):11615-11638. doi: 10.1021/acs.jmedchem.0c00793. Epub 2020 Oct 7. PMID: 33026811; PMCID: PMC8015227.
4 Dalvie D, Xiang C, Kang P, Zhou S. Interspecies variation in the metabolism of zoniporide by aldehyde oxidase. Xenobiotica. 2013 May;43(5):399-408. doi: 10.3109/00498254.2012.727499. Epub 2012 Oct 10. PMID: 23046389.
5 PDB ID: 4UHW. Coelho, C. ,Romao, MJ , Santos-Silva, T. (2015) The Structure of Human aldehyde oxidase doi:10.2210/pdb4UHW/pdb
6 Pike A, Williamson B, Harlfinger S, Martin S, McGinnity DF. Optimising proteolysis-targeting chimeras (PROTACs) for oral drug delivery: a drug metabolism and pharmacokinetics perspective. Drug Discov Today. 2020 Jul 18:S1359-6446(20)30293-2. doi: 10.1016/j.drudis.2020.07.013. Epub ahead of print. PMID: 32693163.
Related Services and Platforms




-

 In Vitro ADME ServicesLearn More
In Vitro ADME ServicesLearn More -

 Novel Drug Modalities DMPK Enabling PlatformsLearn More
Novel Drug Modalities DMPK Enabling PlatformsLearn More -

 Physicochemical Property StudyLearn More
Physicochemical Property StudyLearn More -

 Permeability and Transporter StudyLearn More
Permeability and Transporter StudyLearn More -

 Drug Distribution and Protein Binding StudiesLearn More
Drug Distribution and Protein Binding StudiesLearn More -

 Metabolic Stability StudyLearn More
Metabolic Stability StudyLearn More -

 Drug Interactions StudyLearn More
Drug Interactions StudyLearn More
Stay Connected
Keep up with the latest news and insights.