Introduction
Radionuclides bearing excessive energy can emit particles or rays spontaneously and release energy to achieve the purpose of diagnosis or therapy. However, the shortcomings of radionuclides, such as low stability , uncontrollability, and off-target toxicity, limit their clinical application. Radionuclides are chelated with a chelator and then coupled with peptides through a linker to form peptide-radionuclide conjugates, ensuring the precise delivery of radionuclides to the target. Combined with the excellent tissue penetration and low immunogenicity of peptides, peptide-radionuclide conjugates can achieve the ideal drug delivery, enhancing therapeutic efficiency and reducing side effects associated with systemic toxicity. In recent years, a number of peptide-radionuclide conjugates have been approved by the FDA (Table 1), which play an increasingly important role in the diagnosis and therapy of cancer treatment.
Drug Name | Approval date | Company | Target | Payload | Indication |
68Ga-DOTATATE | June 2016 | Advanced Accelerator Applications S.A/ Novartis | SSTR | 68Ga | Use with PET for localization of somatostatin receptor-positive NETs in adult and pediatric patients |
177Lu-DOTATATE | January 2018 | Advanced Accelerator Applications S.A/ Novartis | Somatostatin recept-or (SSTR) | 177Lu | Somatostatin receptor-positive gastroenteropancreatic neuroendocrine tumors(GEP-NETs) |
64Cu-DOTATATE | September 2020 | RadioMedix | SSTR | 64Cu | Positron emission tomography (PET) for localization of somatostatin receptor NETs in adult patients |
TLX591-CDx | December 2021 | Telix Pharmaceuticals | Prostate-specific membrane antigen (PSMA) | 68Ga | Diagnosis of carcinoma of the prostate |
68Ga-PSMA-11 | December 2020 | Novartis | PSMA | 68Ga | Diagnosis of carcinoma of the prostate |
177Lu-PSMA-617/Pluvicto | March 2022 | Novartis | PSMA | 177Lu | PSMA-expressing metastatic castration-resistant prostate cancer(mCRPC) |
Table 1. The peptide-radionuclide conjugates approved by FDA
The historical development and types of peptide-radionuclide conjugates
Since the 1920s, radionuclides have been used for diagnosis and therapy. 177Lu-DOTATATE, the first peptide-radionuclide conjugate for therapy, was approved in 2018, unveiling the prelude to the rapid development of peptide-radionuclide conjugates. Pharmaceutical companies represented by Novartis have developed multiple pipelines targeting SSTR, PSMA, CXC chemokine receptor 4 (CXCR4), and fibroblast activation protein (FAP) and opened the era of integration of diagnosis and therapy (Figure 1).

PET: Positron Emission Tomography;
CT: Computed Tomography;
18F-FDG: 18F-Fludeoxyglucose;
RGD: (Arg-Gly-Asp) peptides;
Ra: Radium; Y: Yttrium; Ga: Gallium; Lu: Lutecium; I: Iodine。
Figure 1. Nuclear drug development timeline.
Peptide-radionuclide conjugates can be divided into diagnostic and therapeutic radionuclides based on emitted particles and usage.
Diagnosis nuclides include positron-emitting nuclides such as 18F, 68Ga, and 123I, which can be imaged by PET, and γ-emitting nuclides such as 99Tc and 67Ga, which can be scanned by single photon emission computed tomography (SPECT). The physical half-lives of diagnostic radionuclides are usually one to a dozen hours, and the short half-lives help prevent long-term exposure to radiation damage.
Therapeutic nuclides include α particles-emitting nuclides such as 223Ra, 225Ac, and β particles-emitting nuclides such as 90Y, 131I, 177Lu, and 90Sr. Therapeutic nuclides can damage DNA mitochondria and cell membranes directly through radiation. They can also play a bystander effect in inducing the death of adjacent cancer cells through the communication between target cells and adjacent cells. They can also exert an abscopal effect to attack distant tumor cells outside the irradiated field1. These three processes cause oxidative stress, stimulate the secretion of endogenous danger signal factors, and activate the immune system2. The physical half-lives of therapeutic nuclides are usually longer than diagnostic nuclides, varying from one day to a dozen days, to ensure a relatively long residence time in the body for efficacy (Figure 2).

Figure 2. The peptide-radionuclide conjugates classification and corresponding radionuclides.
The selection of radionuclides depends on multiple factors, such as the penetration range, linear energy transfer (LET) of emitters, and physical half-life of particles emitted by radionuclides, combined with the size, type, density, and heterogeneity of tumors (Figure 3) 3. The characteristics and application of emitted particles are summarized in Table 2.

Figure3. Types of radioactive decay and their tissue penetration range3.
Emitted particles | Penetration range | Linear energy transfer | Application |
α particles | 50-100 µm | 80-100 keV/µm | The penetration depth is only a few cell |
β particles | 0.2-8 mm | 0.2 keV/mm | It can penetrate deep into the tumor and can also partially damage the surrounding normal tissues. Common β emitters include 177Lu, 90Y, and 131I, which have been used in treating thyroid cancer. |
Auger particles | 2-500 nm | 4-26 keV/µm | It has high LET, which is suitable for minimizing damage to normal tissues. But auger emitters should be delivered at close proximity to the target cells due to the small penetration depth. |
Positrons emitted from radionuclides with β+ decay | The radionuclides with β+ decay emit positrons that are used exclusively for diagnosis and can be visualized via PET. Common β+ emitters usually have short half-lives (e.g.15O, 13N, 11C, and 18F). | ||
Table 2. The characteristics and application of emitted particles3
Examples of FDA-approved peptide-radionuclide conjugates
Disease background:
Prostate cancer is the second most common cancer in men worldwide. Current treatments include surgery, androgen deprivation therapy, chemotherapy, etc., but the recurrence rate after primary treatment is high (20-60%), with a poor end-stage prognosis. The 5-year survival rate is low (below 30%). Moreover, conventional imaging techniques have a low detection rate and have insufficient performance in describing disease progression4.
Prostate-specific membrane antigen (PSMA) is overexpressed in prostate cancer, and the expression level is 100-1000 fold than that in normal tissues5. It promotes angiogenesis, shows a significant proliferative advantage, and can translocate from the apical to the luminal surface of the prostatic duct, where it becomes accessible on the outside of the cell for binding to ligands6. The expression of PSMA increases with tumor aggressiveness, metastatic disease, and recurrence. So, it is suitable as a molecular target for imaging and therapy. 68Ga-PSMA-11 and 177Lu-PSMA-617 binding to PSMA with high-affinity, realize precise diagnosis and treatment in prostate cancer, respectively.
2.1 Peptide-radionuclide conjugate 68Ga-PSMA-11 for diagnosis
In December 2020, the FDA approved 68 Ga PSMA-11 as the first diagnostic reagent indicated for PET in men with PSMA-positive lesions. The drug consists of a peptide PSMA-11, which targets PSMA, a linker, a chelator, and radionuclide68Ga, and the structure is shown in Figure 4. The clinically recommended dosage is 111 MBq-259 MBq (3 mCi-7 mCi) by intravenous injection. Imaging can be achieved after 50 to 100 minutes post-dose7.

Figure 4. The structure of 68Ga-PSMA-11(targeting peptide in purple, linker in blue, chelator in red, and radionuclide in black).
The peptide PSMA-11 targets and binds to the overexpressed PSMA on prostate cancer cells, and 68Ga emits positron, which is scanned by PET. The physical half-life of 68 Ga is 68 minutes, followed by transformation to stable 68 Zn. It takes only a few hours to complete imaging after administration. 68Ga-PSMA-11 has a considerable detection rate in patients clinically evaluated for prostate cancer metastasis and recurrence (sensitivity 47%, specificity 90%, positive predictive value 61%, and negative predictive value 84% ), and the incidence of adverse effects is low (< 1%) with the most commonly reported adverse reactions being nausea, diarrhea, and dizziness.
Pharmacokinetics of 68Ga-PSMA-11 7:
Binding to PSMA and internalization of 68Ga-PSMA-1:
68 Ga-PSMA-11 is bound to the membrane surface and internalized into the human prostate cancer cell line (LNCaP). The uptake of 68 Ga-PSMA-11 into cells at 37 °C was approximately 2035%, which was higher than that at 4 °C. The binding and internalization of 68 Ga-PSMA-11 were completely blocked when co-incubated with 500 μM of 2-PMPA (a competitive blocker of PSMA).
Distribution of 68Ga-PSMA-11:
68Ga-PSMA-11 intravenously injected was cleared from the blood, and the blood radiation activity showed bi-exponential behavior with half-lives of 6.5 minutes and 4.4 hours, respectively.
In healthy humans, 68 Ga-PSMA-11 preferentially accumulated in the liver (15%), kidneys (7%), spleen (2%), and salivary glands (0.5%). 68Ga-PSMA-11 was also seen in the adrenal glands and prostate. No 68Ga-PSMA-11 uptake was found in the cerebral cortex or heart, and uptake of 68Ga-PSMA-11 in the lungs was usually very low.
In patients with prostate cancer, lymphatic metastasis of prostate cancer in the pelvis can be observed by PET/CT 1 hour after the injection of 170 MBq of 68Ga-PSMA-11 (red arrows in Figure 5a and Figure 5b), and the radiation intensity gradually increased and reached the peak at 4 hours, indicating targeted delivery of 68Ga-PSMA-11 in prostate cancer lesions.

Figure 5. Sequential PET/CT of a Patient Following the Injection of 170 MBq 68Ga-PSMA-11.
Metabolism of 68Ga-PSMA-11:
After internalization of the ligand-bound receptor, the ligand dissociated from the receptor and was degraded by proteolytic enzymes into amino acids. 67Ga-PSMA-11 was stable after 48 hours of incubation at 37 ℃ in human serum, and no free 67Ga was detected8. Incubation of 68Ga-PSMA-11 in the presence of excess amount of transferrin at 37℃ for 2 hours, 68Ga was notchelated to transferrin.
Excretion of 68Ga-PSMA-11:
68Ga-PSMA-11 was primarily excreted via the kidneys.
Drug interactions of 68Ga-PSMA-11:
The PSMA blockers like 2-PMPA can potentially inhibit the binding and cellular internalization of 68Ga-PSMA-11 to PSMA. However, there is no clinical concern currently, given that no approved drugs currently contain PSMA blockers7.
2.2 Peptide-radionuclide conjugate 177Lu-PSMA-617 for therapy
In March 2022, the FDA approved 177 Lu-PSMA-617 as a radioligand therapy targeting PSMA. 177Lu-PSMA-617 consists of a peptide PSMA-611, which targets PSMA, a linker, a chelator, and radionuclide 177Lu, and the structure is shown in Figure 6. It is the first radioligand therapy -approved by the FDA to treat patients with metastatic trend-resistant prostate cancer and has received breakthrough therapy designation. The results of the phase III clinical study showed that the combination therapy (BSC/BSoC + 177Lu-PSMA-617) can prolong the radiographic progression-free survival and overall survival of patients by about 4 months compared with BSC/BSoC standard therapy9.

Figure 6. The structure of 177Lu-PSMA-617 (targeting peptide in purple, linker in blue, chelating agent in red, and radionuclide in black).
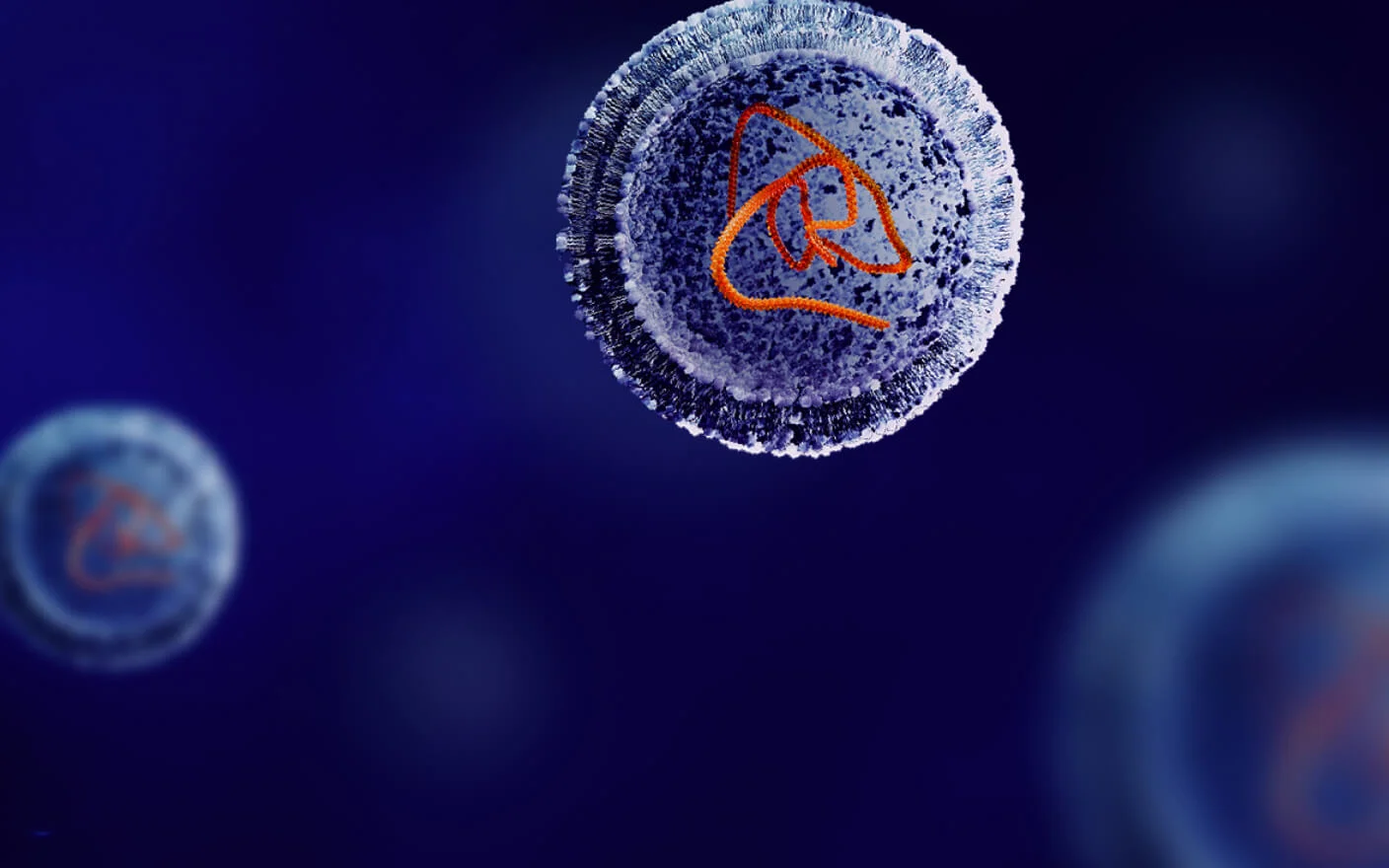
After entering the body, 177Lu-PSMA-617 binding to PSMA overexpressed on the surface of prostate cancer cells is internalized into the tumor cells via clathrin-mediated endocytosis and transported intracellularly via endosomes. The antigen PSMA is recycled to the cell membrane surface or degraded by lysosomal enzymes. 177Lu is released and emits β-particles to kill cancer cells (Figure 7) 10.

Figure 7. Schematic model of 177Lu-PSMA-617 internalization.
The advantage of 177Lu
The β-rays emitted by 177Lu can not only exert cell killing directly, but also induce oxygen free radicals to break DNA.
The average penetration range of β-rays emitted by 177Lu is 0.28 mm in the tissue, which can play a crossfire effect to destroy the surrounding tumor cells that do not express the specific antigen. Combined with the targeting components, 177 Lu can precisely kill tumors and overcome tumor heterogeneity.
177Lu can produce γ photon with an emission energy of 208.4 keV, which can be used for SPECT imaging, integrating diagnosis and therapy.
177Lu, with a physical half-life of 6.7 days, is more stable and less volatile than 131I.
Pharmacokinetics of 177Lu-PSMA-617:
Distribution of 177Lu-PSMA-617:
The geometric mean distribution volume of PSMA-617 was 123 L. Unlabeled PSMA-617, and non-radioactive 175Lu-PSMA-617 showed moderately bound (approximately 60%-70%) with human plasma. The human blood plasma partitioning ratio were both less than 1, indicating PSMA-617 and 175Lu-PSMA-617 are not distributed into human erythrocytes specifically.
In healthy humans, 177Lu-PSMA-617 is mainly distributed in the gastrointestinal tract, liver, lungs, kidneys, heart wall, bone marrow, and salivary glands within 2.5 hours of intravenous administration.
After administration of one to two cycles of 177Lu-PSMA-617 to patients with low, low to intermediate, intermediate to high, and high prostate tumor load, 177Lu-PSMA-617 showed strong targeting to prostate cancer metastases and low accumulation in other tissues (Table 3) 11.
Tumor load | Low (Patient 1) | low to Intermediate (Patient 2) | Intermediate to high (Patient 3) | High (Patient 4) | ||||
1st cycle | 2nd cycle | 1st cycle | 2nd cycle | 1st cycle | 2nd cycle | 1st cycle | 2nd cycle | |
Kidney | 0.55 | 0.56 | 1.14 | 0.82 | 0.81 | 0.76 | 0.62 | 0.76 |
Red marrow | 0.02 | 0.02 | 0.02 | 0.02 | 0.03 | 0.03 | 0.05 | 0.03 |
Parotid gland | 2.2 | 1.16 | 1.03 | 0.82 | 1.26 | 1.3 | 1.27 | 1.17 |
Submandibular gland | 1.3 | 1.69 | 1.26 | 0.97 | 1.37 | 1.31 | 1.82 | 2.13 |
Liver | 0.09 | 0.1 | 0.07 | 0.06 | 0.09 | 0.1 | 0.16 | 0.13 |
Spleen | 0.19 | 0.15 | 0.26 | 0.14 | 0.11 | 0.13 | 0.28 | 0.27 |
Bladder wall | 0.03 | 0.16 | 0.16 | 0.17 | 0.29 | 0.23 | 0.41 | 0.36 |
Metastasis (mean) | 6.1 | 22.8 | 15.3 | 14 | ||||
Table 3.Organ dosimetry of 4 patients with prostate cancer during their first and second cycles of 177 Lu-PSMA-617(Gy/GBq)
Note: Tumor load refers to the number of cancer cells and tumor size.
Metabolism of 177Lu-PSMA-617:
175Lu-PSMA-617 and PSMA-617 were stable in the plasma from humans, rats, and minipig for up to 2 hours at 37℃. 175Lu-PSMA-617 and PSMA-617 were stable in the liver and kidney S9 fractions from human, rat, and minipig for up to 1 hour at 37℃.
Excretion of 177Lu-PSMA-617:
In humans, the terminal elimination half-life of 177Lu-PSMA-617 was about 41.6 hours. The total systemic clearance (CL) was 2.04 L/h, and 177Lu-PSMA-617 was primarily eliminated via the kidneys as intact. Only 1%-5% of the injected radioactivity was detected in feces.
Drug Interaction of 177Lu-PSMA-617:
Interactions with metabolic enzymes: 177Lu-PSMA-617 and PSMA-617 were not inhibitors for CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6 and 3A, and were not inducers of CYP1A2, 2B6 and 3A4. PSMA-617 was not a substrate of CYP450s.
Interactions with transporters: PSMA-617 was not a substrate of BCRP, P-gp, MATE1, MATE2-K, OAT1, OAT3 and OCT2 in vitro; PSMA-617 was not an inducer of BCRP, P-gp, MATE1, MATE2-K, OAT1, OAT3, OATP1B1, OATP1B3, OCT1 and OCT2 in vitro 9.
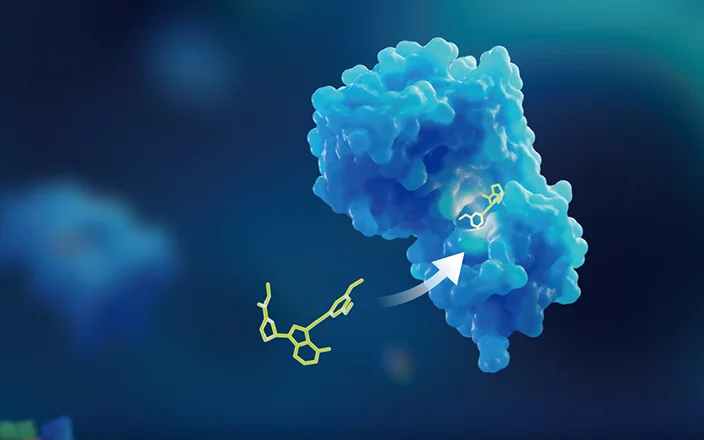
Characteristics of ideal peptide-radionuclide conjugates (Figure 8)
Appropriate ray types and emission energy: Radionuclides used for diagnosis normally emit γ rays or positrons (β +), preferably no or less emission of β- and α-rays to reduce radiation damage. Radionuclides used for therapy normally emit α or β- rays mostly and no or less γ rays to improve the therapeutic effect. The emission energy of β- is recommended to be lower than 1 MeV, and the counterpart for α is recommended to be lower than 6 MeV.
Appropriate physical half-lives: The ideal physical half-lives of radionuclides are normally in the range of 30 minutes to 10 days. On the premise of successful imaging, the physical half-lives of diagnostic radionuclides should be as short as possible to reduce the exposure time in vivo to protect patients from radiation. The physical half-life of therapeutic radionuclides should not be too short, generally 1 to 10 days, to ensure efficacy.
Low toxicity: The radionuclides and their decay products should have little or no toxicity. The decay products are preferably stable nuclides.
Stable linkers: Non-cleavable linkers are generally used to enhance stability and decrease off-target risks.
Target specificity: Peptide-radionuclide conjugates emit radiation once administered. Therefore, high specificity of the target and low accumulation in non-specific tissues are preferred.

Figure 8. Characteristics of an ideal peptide-radionuclide conjugates.
DMPK strategies for peptide-radionuclide conjugates
Many DMPK studies could be carried out with cold counterparts that are not radioactive, such as conjugates containing stable isotopes or the decay products from radionuclides, due to the high threshold for radioisotope experiments if the nuclides are already in clinical use12. Of course, DMPK studies could be carried out directly with radioactive conjugates if the condition is allowed.
Generally, peptides are easily degraded by proteases, so the stability of peptide-radionuclide conjugates in matrices like plasma, liver S9, kidney homogenate, and so on is essential for DMPK research. Meanwhile, the structure will be optimized based on in vivo and in vitro metabolite identification studies. Plasma protein binding, whole blood to plasma partitioning, and rodent PK with peptide or cold conjugates help to further understand the disposition of peptide-radionuclide conjugates. In addition, it is also necessary to pay attention to the interaction of drugs with metabolic enzymes and transporters.
Tissue distribution in rodents or large animals, or model animals with hot conjugates are useful for studying organ distribution and is beneficial to predict the dosage for first in human studies. Excretion study in rodents with the hot conjugate facilitates understanding of mass balance and excretion pathway.
The DMPK strategies of peptide-radionuclide conjugates for pre-clinical studies and IND-enabling studies are summarized in Table 4.
DMPK | Assays |
In vitro studies | 1. Stability in blood, plasma (suggest heparin as anticoagulation), liver S9, kidney homogenate with peptide or cold conjugates 2. Metabolite profiling/identification in blood, plasma, liver S9, and kidney homogenate with peptide or cold conjugates 3. Plasma and tissue protein binding (ultracentrifuge method), blood to plasma partitioning with peptide or cold conjugates 4. Drug interaction between enzymes and transporters with peptide or cold conjugates |
In vivo studies | 1. PK in rodent and non-rodent under clinical administration route with peptide or cold conjugates 2. The bioanalytical method development and qualification in plasma (for IND-enabling) 3. Tissue distribution with hot compound 4. Mass balance with hot compound |
Table 4. DMPK Strategies of peptide-radionuclide conjugates
Conclusion:
The global radiopharmaceutical market is in a stage of rapid development and is expected to reach 10 billion dollars by 2030. The increased incidence of cancer also raises the need for radiopharmaceuticals. With more pipelines from pharmaceutical companies combining the facilitation from regulatory agencies and governments, the global enthusiasm for research and development of peptide-radionuclide conjugates is unprecedented, which leads the diagnosis and therapy of cancer into a whole new era.
Talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Authors: Chong Chen, Qigan Cheng, Jing jin
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,600+ global clients, and have successfully supported 1,500+ IND applications.
Reference
1.Shiraishi, K. (2012). Abscopal effect of radiation therapy: current concepts and future applications. Modern Practices in Radiation Therapy.
2.Rondon, A., Rouanet, J., & Degoul, F. (2021). Radioimmunotherapy in oncology: overview of the last decade clinical trials. Cancers, 13(21), 5570.
3.Peltek, O. O., Muslimov, A. R., Zyuzin, M. V., & Timin, A. S. (2019). Current outlook on radionuclide delivery systems: from design consideration to translation into clinics. Journal of nanobiotechnology, 17, 1-34.
4.Bois, F., Noirot, C., Dietemann, S., Mainta, I. C., Zilli, T., Garibotto, V., & Walter, M. A. (2020). [68Ga] Ga-PSMA-11 in prostate cancer: a comprehensive review. American Journal of Nuclear Medicine and Molecular Imaging, 10(6), 349.
5. Yao, V., Berkman, C. E., Choi, J. K., O'Keefe, D. S., & Bacich, D. J. (2010). Expression of prostate‐specific membrane antigen (PSMA), increases cell folate uptake and proliferation and suggests a novel role for PSMA in the uptake of the non‐polyglutamated folate, folic acid. The Prostate, 70(3), 305-316.
6.Bouchelouche, K., Turkbey, B., & Choyke, P. L. (2016, November). PSMA PET and radionuclide therapy in prostate cancer. In Seminars in nuclear medicine (Vol. 46, No. 6, pp. 522-535). WB Saunders.
7.http://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/212642Orig1s000MutlidisciplineR.pdf
8.Eder, M., Neels, O., Müller, M., Bauder-Wüst, U., Remde, Y., Schäfer, M., ... & Kopka, K. (2014). Novel preclinical and radiopharmaceutical aspects of [68Ga] Ga-PSMA-HBED-CC: a new PET tracer for imaging of prostate cancer. Pharmaceuticals, 7(7), 779-796.
9.http://www.accessdata.fda.gov/drugsatfda_docs/nda/2022/215833Orig1s000MultidisciplineR.pdf
10.Heesch, A., Maurer, J., Stickeler, E., Beheshti, M., Mottaghy, F. M., & Morgenroth, A. (2020). Development of radiotracers for breast cancer—the tumor microenvironment as an emerging target. Cells, 9(10), 2334.
11.Kratochwil, C., Giesel, F. L., Stefanova, M., Benešová, M., Bronzel, M., Afshar-Oromieh, A., ... & Haberkorn, U. (2016). PSMA-targeted radionuclide therapy of metastatic castration-resistant prostate cancer with 177Lu-labeled PSMA-617. Journal of Nuclear Medicine, 57(8), 1170-1176.
12. 放射性体内诊断药物非临床评价技术指导原则 2021年2月。
13.药物免疫原性研究技术指导原则 2021年3月。
Related Services and Platforms




Stay Connected
Keep up with the latest news and insights.