Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than one billion people worldwide since the emergence of the pandemic in late 2019. In February 2020, the disease caused by the SARS-CoV-2 was officially named coronavirus disease (COVID-19). With the persistent spread of SARS-CoV-2, mutated virus strains have continuously emerged, ranging from the Alpha variant and the Delta to the Omicron variants that spread globally. These viral variants have led to recurrent global COVID-19 outbreaks. COVID-19 vaccines, as a crucial weapon against the pandemic, have gained public attention and discussion. This article introduces the progress in vaccine development and relevant applications of mRNA vaccines during the COVID-19 pandemic. Additionally, it discusses the methods for conducting pharmacokinetic (PK) studies on mRNA vaccines based on the interpretation of relevant guidelines.
The overview of vaccine development throughout the COVID-19 pandemic
(1) Pathogenesis of COVID-19
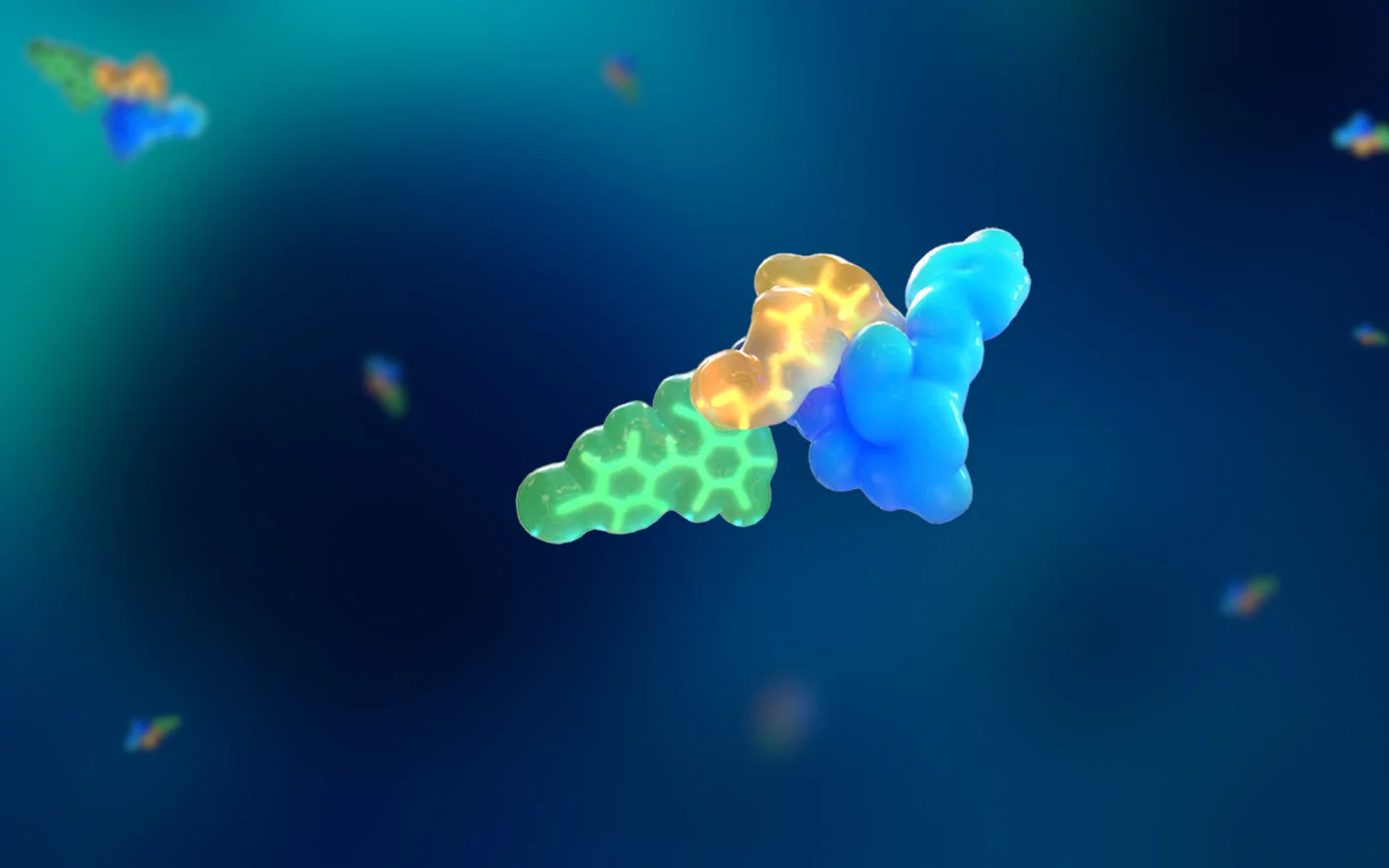
SARS-CoV-2 infection mode is mainly through the respiratory tract, and the most serious disease that it can potentially cause in humans is pneumonia. The virus can infect humans through the mucous membranes of the mouth, nose, and eyes, and migrate along the upper respiratory trachea to reach the lower respiratory tract, eventually reaching the lungs. When the virus reaches the alveoli, the spike (S) protein present in the virus binds to the ACE2 receptor on type II alveolar cells, allowing the virus to enter the cells through endocytosis. The virus then releases RNA to seize control of the function of the original cell and achieve massive replication. After fully utilizing the cell’s replicative capacity, the virus causes the cell to rupture, releasing viral particles that infect surrounding type II alveolar cells (Figure 1).1 After sufficient exposure to the virus, the adaptive immune system of the body becomes activated. In the process of attacking infected tissues, the immune system also kills healthy alveolar cells, resulting in impaired gas exchange and reduced respiratory function. Severe cases may lead to acute respiratory distress syndrome and even death.

Figure 1. Schematic diagram of cellular entry and exit of SARS-CoV-2.1
(2) Mechanism of action of vaccines
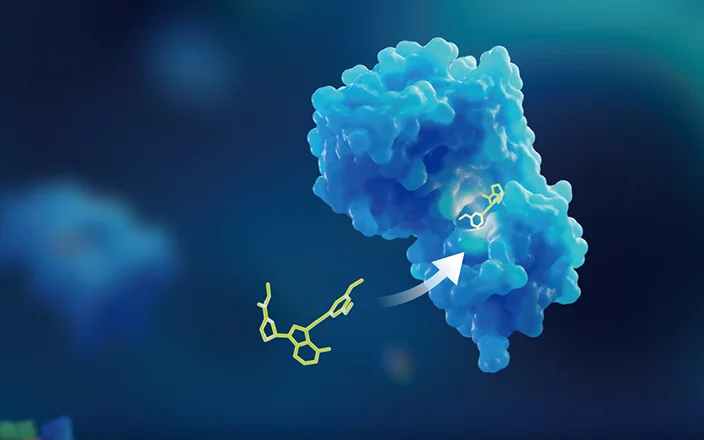
Vaccines use pathogenic material to stimulate the immune system to produce specific memory B and T cells. When the body is attacked by the same pathogen in the future, the acquired immunity of the body will use immunological memory to produce a rapid response, killing the pathogen and the infected cells before large-scale infection takes place. The S protein, which is involved in the pathogenesis of COVID-19, has been used as an antigen in vaccine development.
(3) Analysis of the advantages and disadvantages of different types of vaccines
Currently, the types of vaccines designed and developed to ameliorate SARS-CoV-2 pathogenesis include inactivated virus vaccines, recombinant protein subunits, adenovirus vector vaccines, and mRNA vaccines.
Inactivated vaccines are developed by growing the pathogen in a specific culture medium and then rendering the virus non-replicative through physical or chemical methods while preserving its antigenicity. These vaccines have the advantage of simple and fast preparation, and they are relatively safe. They are commonly used for combating acute disease transmission. However, their disadvantages include a single immunization route, the need for a large-scale culture of the virus under P3 conditions, and the potential for antibody-dependent enhancement which can exacerbate viral infections.
Recombinant protein subunit vaccines involve inserting gene segments from the pathogen’s genome that encode “effective antigenic components” into the genome of host cells. These host cells then express the required antigenic components in vitro. This vaccine does not involve live pathogens in the production process, thus eliminating the risk of pathogen leakage. Additionally, host cells can be rapidly mass-produced through industrial fermentation and similar techniques, thereby providing this method with substantial cost and efficiency advantages.
Adenovirus vector vaccines are produced by inserting genes that express specific antigens of a virus into the genome of a non-replicable adenovirus through recombination, express the desired antigens in human cells. This type of vaccine causes few adverse reactions and is easy to produce on a large scale. However, most people have been exposed to different types of adenoviruses, which could result in the presence of antibodies that can neutralize the adenoviral vector, leading to reduced vaccine efficacy.
mRNA vaccines involve directly injecting modified mRNA encoding pathogen-specific antigens into the human body after certain processing steps, allowing the body’s protein synthesis system to produce the desired antigens. This type of vaccine does not involve live pathogens in the production or vaccination processes, which eliminates the risk of virus spread and infection. mRNA vaccines can also target the expression of specific antigens, avoiding the adverse effects that other components of pathogens can impose on the human body. Furthermore, it involves “infection” of the cells, which can trigger both humoral and cellular immunity. However, the application of this vaccine technology has a shorter development timeline compared to other vaccine technologies and thus requires extensive validation.
(4) Approved and emergency authorized COVID-19 vaccines
There are currently multiple COVID-19 vaccines following different technological pathways approved and granted emergency authorization for use globally, following different technological pathways. As of the end of 2022, 13 COVID-19 vaccines have been approved or authorized for emergency use in China. These vaccines have shown different protective effects during the clinical phase. According to public phase III trial data, several inactivated virus and adenovirus vector vaccines displayed protective efficacies between 50% and 85%, while the mRNA vaccines developed by both Pfizer/BioNtech and Moderna have exhibited protection rates exceeding 90%.2,3 These mRNA vaccines play an important role in controlling the global outbreak of COVID-19. As SARS-CoV-2 continues to mutate, the Pfizer/BioNtech mRNA vaccine has also been studied for protection against mutant strains. The efficacy of two doses of the Pfizer/BioNtech mRNA vaccine against the Delta strain is reportedly 88% in England,4 79% in Scotland,5 and 87% in Canada.6 The efficacy of protection against the Omicron variant was reported to be 75.5% in England.7 The protection may have been derived from cellular immunity. Studies have shown that most T-cell responses are generated by invariant epitopes between the prototype B-lineage virus and the variant of concern.8
The ongoing COVID-19 pandemic has highlighted the importance of vaccines and the urgent global demand for them. mRNA vaccines have gained attention worldwide, and their potential for application in other fields needs to be paid attention to.
Application prospects for mRNA vaccines
Theoretically, mRNA can express any protein to treat a wide range of diseases, making it a highly promising technology platform. From 2003 to 2020, more than 140 mRNA vaccines have been used in clinical trials involving a variety of disease areas, including cancer and infectious diseases (Figure 2). This demonstrates the increasing application and attention given to mRNA vaccines in various fields.

Figure 2. Number of clinical trials using mRNA vaccines summarized by disease type (left) and delivery system (right).9
(1) mRNA vaccines against infectious diseases
Developing preventive or therapeutic vaccines targeting infectious pathogens is the most effective means of controlling and preventing epidemics. The commercial vaccine development and approval process for traditional vaccines is slow, which makes it challenging to address rapidly emerging acute viral diseases. As a consequence, mRNA vaccines have garnered increased attention owing to their short development cycles and simple production processes. Currently, mRNA vaccine development primarily focuses on SARS-CoV-2, human immunodeficiency virus, and rabies. With the approval of mRNA vaccines for COVID-19, the feasibility of the mRNA technology platform in the vaccine field has been validated.
(2) mRNA vaccines against cancer
Cancer vaccines and other immunotherapies represent new strategies for treating malignant tumors. These vaccines use tumor antigens to induce the immune response of the body against tumor cells in a specific manner. mRNA vaccines activate cellular immunity. T cells target tumor cells with a high killing efficiency. The production of antigen types and sequences can be precisely controlled by editing the mRNA sequence. Specific antigen protein markers that are only secreted in tumor cells can be selected as targets, avoiding damage to normal cells and enabling more precise targeting of specific immune targets. Currently, over 50% of clinical trials in mRNA vaccine development are focused on the treatment of melanoma, prostate cancer, and brain cancer (Figure 3), with most trials still in the early stages (Phase I and II).
In summary, as the number of clinical trials for mRNA vaccines and the range of applications continues to increase, along with the approval of mRNA COVID-19 vaccines, the mRNA vaccine technology is continuously evolving and showing promising prospects for development.

Figure 3. Number of clinical trials and application areas for mRNA vaccines.9
Insight into the DMPK studies for mRNA vaccine development
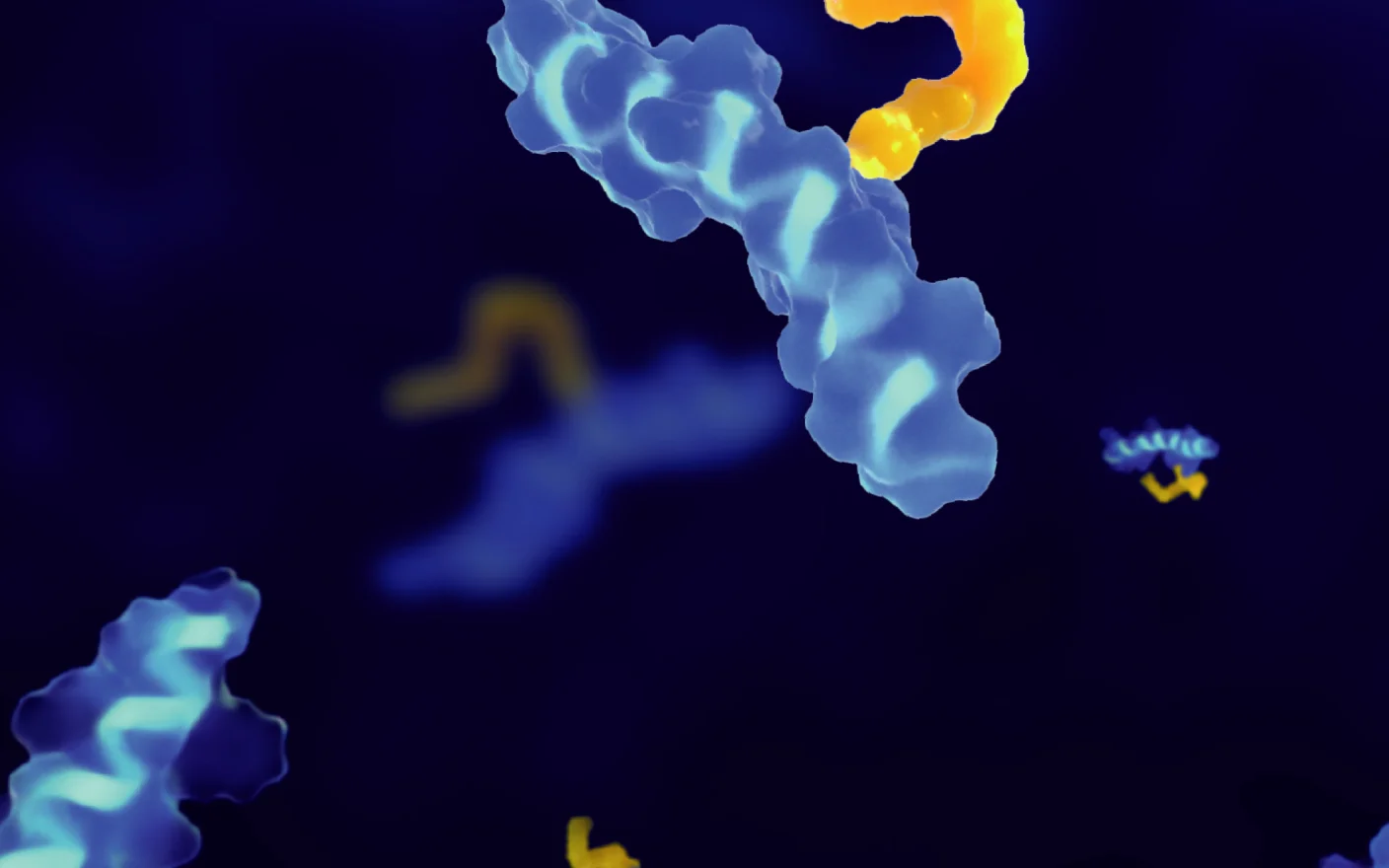
mRNA vaccines are a class of nucleic acid vaccines in which a partial mRNA fragment from a virus is synthesized in vitro and injected into human cells to produce the corresponding antigen, which stimulates the specific immune response of the body and produces relevant immune memory (Figure 4). The entry of intact mRNA into the cytoplasm is pivotal to vaccine function. However, the single-stranded structure of mRNA makes it highly unstable and susceptible to degradation. mRNA is a large molecule carrying a negative charge, posing a challenge in its delivery across the cell membrane composed of anionic lipids. Therefore, special modifications or encapsulation delivery systems are required to achieve intracellular expression of mRNA.

Figure 4. Mechanism of action of mRNA vaccines.10
Lipid nanoparticles (LNPs) are one of the most commonly used tools for mRNA delivery. This delivery system is used for both currently approved mRNA vaccines for SARS-CoV-2. LNPs refer to a class of lipid particles, including lipid gels and liposomes. In April 2018, the Food and Drug Administration (FDA) issued guidance on the use of liposomal drugs,11 highlighting the need for studying their PK and mass balance and identifying information, such as the major metabolites associated with the therapeutic and toxic effects. In August 2021, the National Medical Products Administration published Technical Guidelines for Non-Clinical PK Studies of Nanomedicines (Trial),12 highlighting the need to study the in vivo release rate and distribution of particles and the PK characteristics of new excipients or carrier materials.
The liposomal-siRNA drug (Onpattro) which was approved in 2018 underwent adequate preclinical DMPK studies, which involved studies on siRNA (ALN-18328) and components of the LNP, including DLin-MC3-DMA and PEG2000-C-DMG. This included investigating the distribution of 14C-labeled DLin-MC3-DMA in rats using the QWBA (quantitative whole-body autoradiography) technique, as well as studying the metabolism and excretion of Onpattro and the LNP component (DLin-MC3-DMA) using 14C-labeled DLin-MC3-DMA. 13
Therefore, before mRNA vaccine formulations are used in healthy populations, comprehensive risk assessments should be conducted, including assessments of both the mRNA and the delivery system. The presence time of mRNA, as the substance generating antigenic proteins, in the body can impact the effectiveness of antibodies. It is imperative to conduct comprehensive research on the absorption, metabolism, and excretion properties of LNPs, as exogenous agents in delivery systems, within the human body. The distribution, metabolism, and excretion of mRNA vaccines and their LNP components can be studied using radiolabeling techniques.
Conclusion
mRNA vaccines have advantages such as safety, efficacy, and high production efficiency. In recent years, there has been an upward trend in the number of clinical trials for mRNA vaccines, covering various therapeutical areas, such as infectious diseases and oncology. With the approval of mRNA vaccines for COVID-19, the applicability of the mRNA technology platform in the vaccine field has been validated, resulting in a growing focus on mRNA vaccines. Although the development of mRNA vaccines faces many challenges, continuously emerging delivery methods will lead to breakthroughs in mRNA vaccine research. The development of cancer vaccines offers new potential for treating malignant tumors and instills hope in a larger number of patients.
If you want to learn more details about the strategies for mRNA, please talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Authors: Ming Tang, Tingting Cai, Lingling Zhang, Weiqun Cao
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing and Nantong), 1,000+ scientists and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,500+ global clients, and have successfully supported 1,200+ IND applications.
Reference
[1] Megan Scudellari. How the coronavirus infects cells — and why Delta is so dangerous. Nature. Vol 595, 29 July 2021.
[2] COMIRNATY® (COVID-19 Vaccine, mRNA) suspension for injection, for intramuscular use Initial U.S. Approval: 2021
[3] http://www.fda.gov/media/153089/download
[4] medRxiv preprint doi: http://doi.org /10.1101/2021.05.22.21257658
[5] http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01358-1/fulltext
[6] medRxiv preprint doi: http://doi.org /10.1101/2021.06.28.21259420
[7] medRxiv preprint doi: http://doi.org/10.1101/2021.12.14.21267615
[8] Pinja Jalkanen, Pekka Kolehmainen, Hanni K. Häkkinen, et al. COVID-19 mRNA vaccine induced antibody responses against three SARS-CoV-2 variants. NATURE COMMUNICATIONS, (2021), 12:3991. http://doi.org/10.1038/s41467-021-24285-4
[9] Sara Sousa Rosa, Duarte M.F. Prazeres, Ana M. Azevedo, et al. mRNA vaccines manufacturing: Challenges and bottlenecks. Vaccine, 39 (2021), 2190–2200. http://doi.org/10.1016/j.vaccine.2021.03.038
[10] Namit Chaudhary, Drew Weissman, Kathryn A. Whitehead. mRNA vaccines for infectious diseases: principles, delivery and clinical translation. Nature Reviews Drug Discovery volume, 20, pages817–838 (2021)
[11] CDER, FDA. Guidance for Industry: Liposome Drug Products: Chemistry, Manufacturing, and Controls; Human Pharmacokinetics and Bioavailability; and Labeling Documentation. 2018. http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm
[12] NMPA. 纳米药物非临床药代动力学研究技术指导原则(试行), 2021.
[13] EMA. Onpattro-epar-public-assessment-report. 2018.
[14] Thi, T.T.H., Suys, E.J.A., Lee, J.S., et al. Lipid-Based Nanoparticles in the Clinic and Clinical Trials: From Cancer Nanomedicine to COVID-19 Vaccines. Vaccines, 2021, 9, 359. http://doi.org/10.3390/vaccines9040359.
Related Services and Platforms




Stay Connected
Keep up with the latest news and insights.