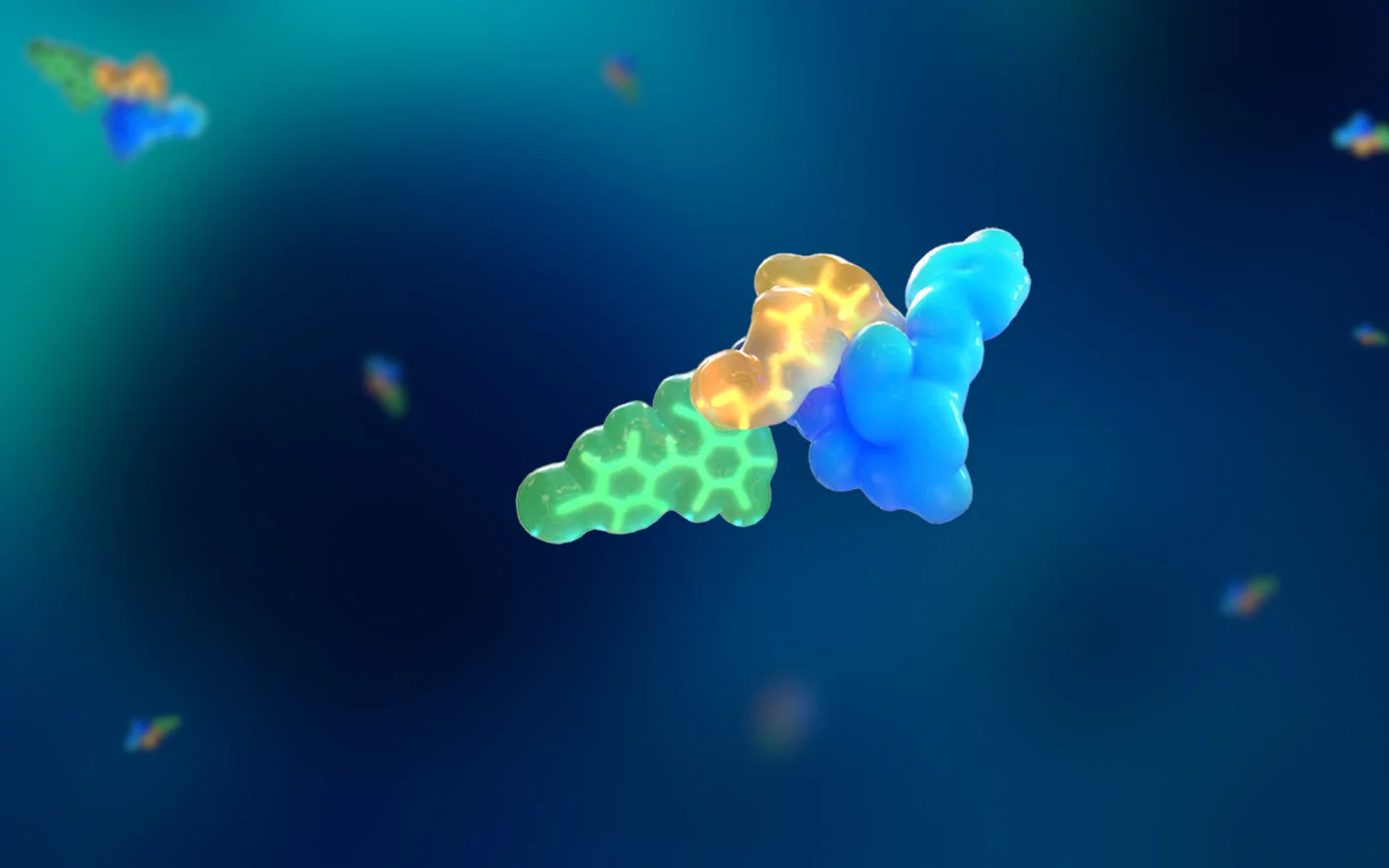
Antibody-drug conjugates (ADCs) are complex molecules composed of a targeting antibody (usually directed at cancer cells), a toxic payload, and a linker. This design aims to deliver the toxic payload with greater precision, minimizing damage to normal cells. Compared to traditional chemotherapy drugs, ADCs offer higher specificity and a wider therapeutic window. The development of ADCs for various tumor indications is rapidly advancing, promising to usher in a new era of precision chemotherapy. This article outlines the key considerations in ADC development and focuses on the preclinical pharmacokinetics and pharmacodynamics (PK/PD) studies.
Key considerations in ADC development
The complexity of ADC structures introduces several critical factors for their development and optimization:
Antigen target: This involves assessing the expression profile of antigens in cancer versus normal cells, the endocytosis mediated by the antigen, and the affinity of the antigen (high expression can lead to binding site obstruction).
Antibody backbone: Considerations include the functionality mediated by receptors such as FcγR and FcRn.
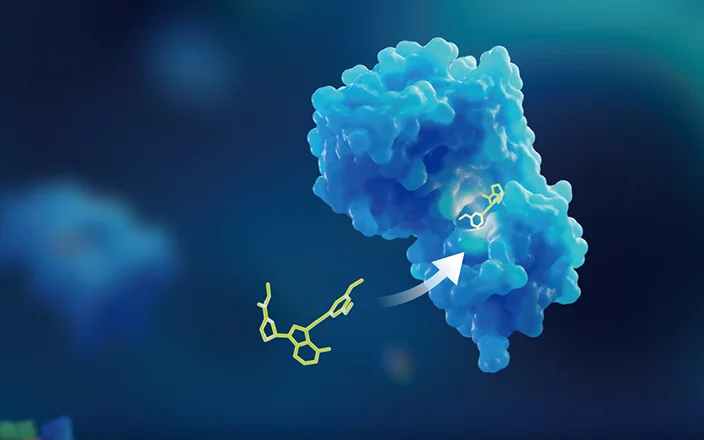
Payload: Factors include toxicity, mechanism of action, half-life, polarity (lipophilicity), and efflux transporters. Typically, payload choices are conservative, often selecting well-studied toxin families like calicheamicins, auristatins, maytansinoids, topoisomerase I inhibitors, and pyrrolobenzodiazepines.
Conjugation site: This must consider the number of payloads conjugated, the type of conjugation (site-specific or non-site-specific), and the uniformity of the drug-to-antibody ratio (DAR).
Linker: Factors include the release mechanism of the payload (cleavable or non-cleavable), hydrophilicity/hydrophobicity, and the site of release (lysosomal or tumor microenvironment).

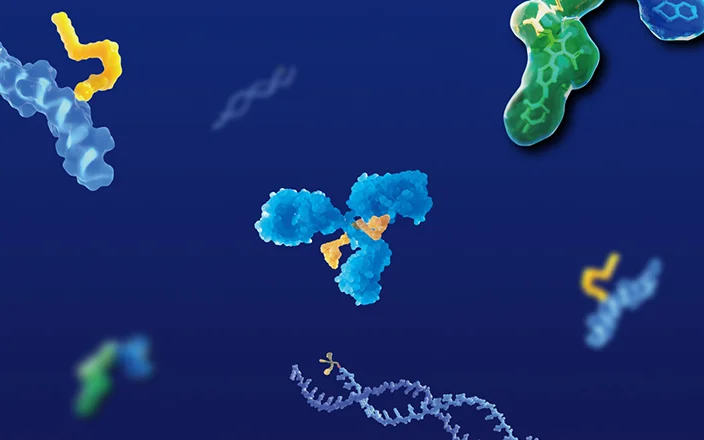
Figure 1. Schematic diagram of the main considerations in ADC drug development.
Preclinical PKPD study of ADC drugs
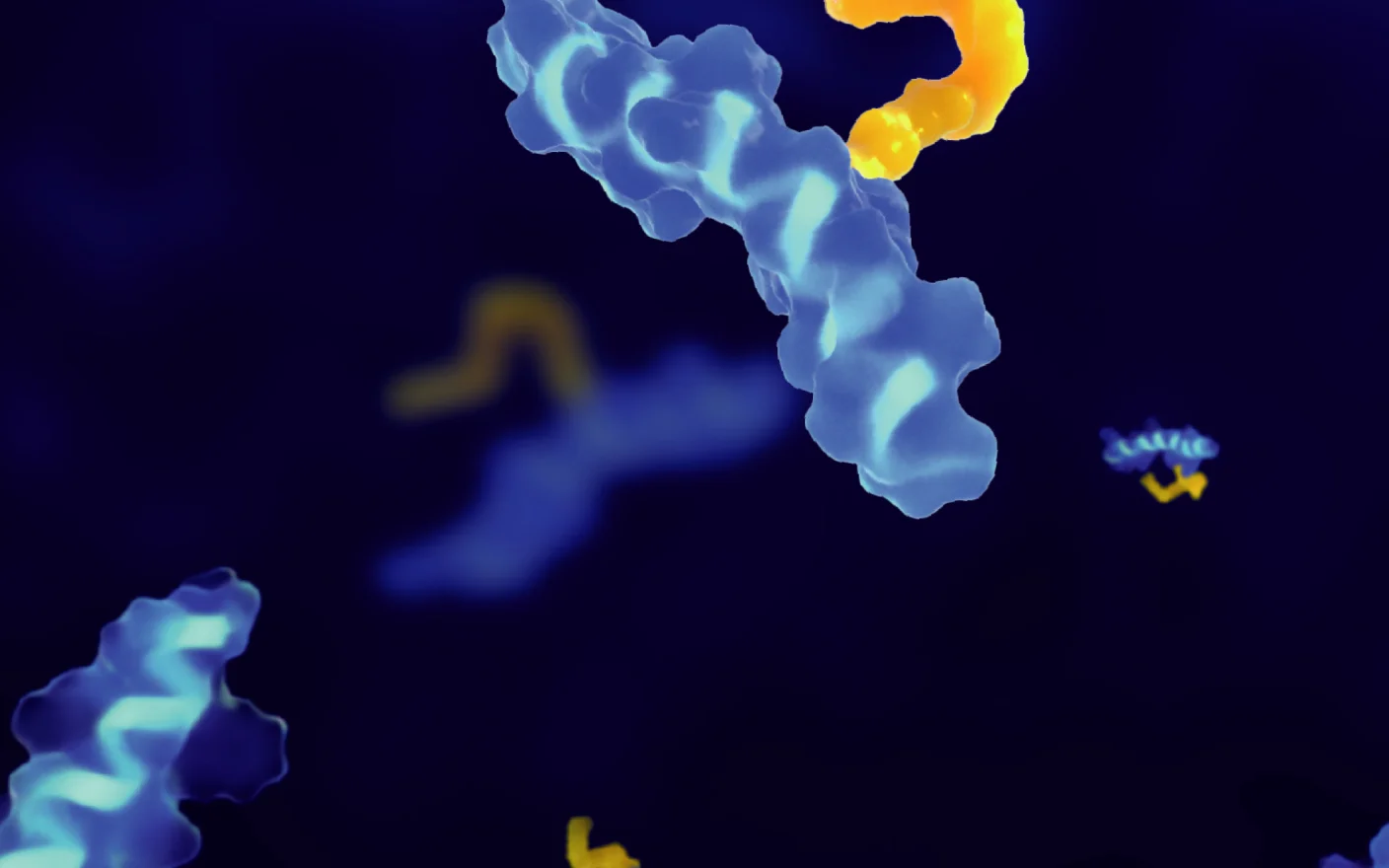
Preclinical pharmacodynamics (PD) studies of ADCs primarily focus on the drug's effects in vitro on cell models and in vivo on animal tumor models. The pharmacokinetics (PK) of ADCs examine their absorption, distribution, metabolism, and excretion (ADME) characteristics in vitro or within animal models. The integration of PK and PD studies allows researchers to explore the dose-response relationship, summarizing and analyzing the behavior and effects of ADCs through empirical or mathematical models.
Due to the complexity of ADC components and mechanisms of action, the PK/PD studies of ADCs present unique characteristics and challenges. For example, the PK profiles may reflect both antibody and small molecule properties, necessitating a quantitative understanding of various molecular forms (such as ADC conjugates, total antibodies, and free payloads). The efficacy of ADCs largely depends on the concentrations of free small payloads and active metabolites within tumor cells. Additionally, the presence of various pharmacological mechanisms (target effects, bystander effects) requires a comprehensive approach in PD studies [1].
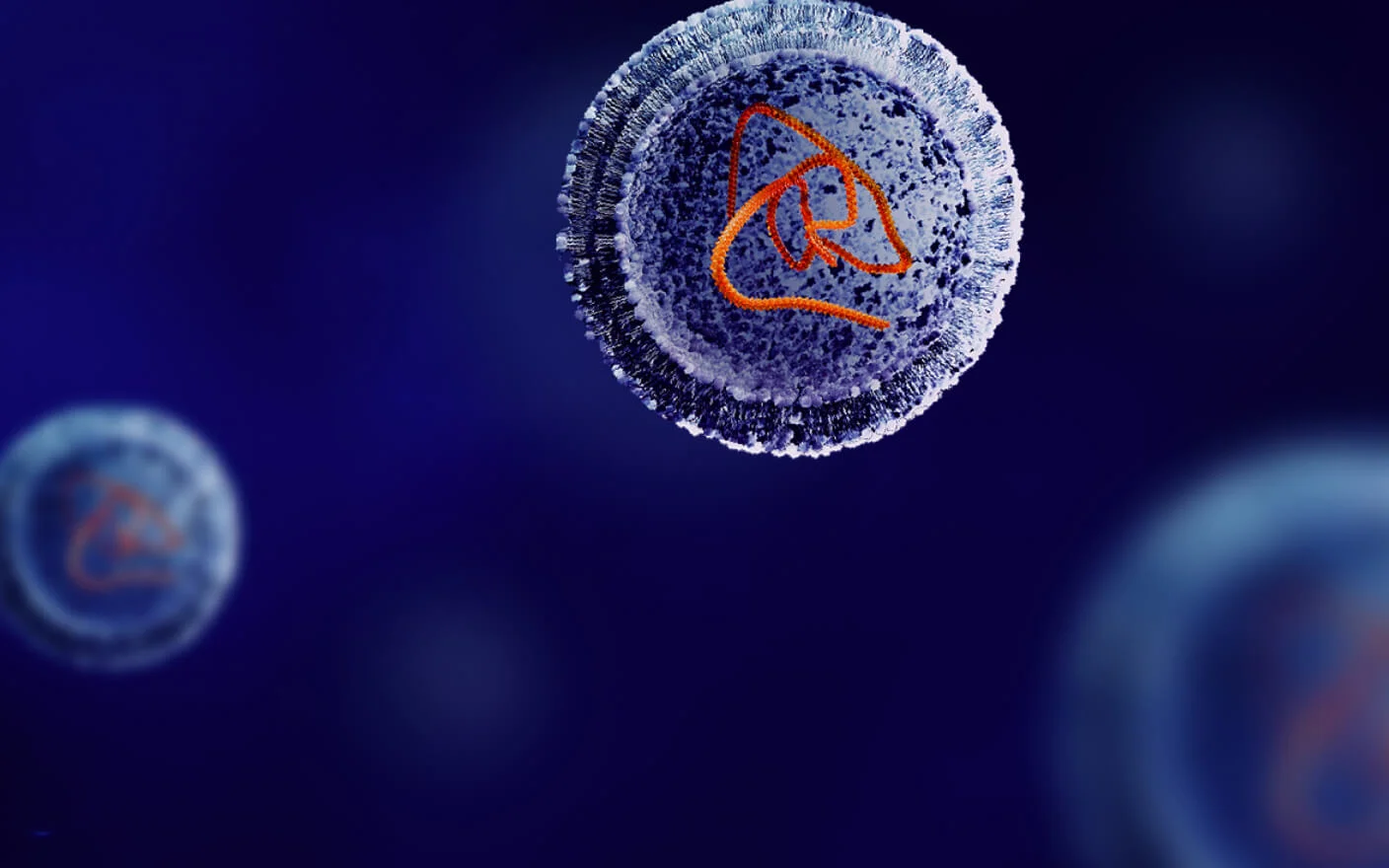
The pharmacokinetic and pharmacodynamic studies recommended for preclinical ADC drugs are listed in Figure 2. The preclinical PK study mainly includes in vitro stability studies, in vivo PK, and tissue distribution studies. In vitro stability studies are often critical for the early development of ADC drugs, and the study of the stability and metabolite identification (Met ID) of ADC drugs in plasma/whole blood systems, lysosomes or acidified liver S9 and liver homogenate systems or tumor cell systems can assist in the understanding of the pharmacological efficacy and potential safety risks of ADC drugs. In vivo PK and tissue distribution studies can help characterize the in vivo ADME profiles of ADC drugs and the exposure levels of different drug components (e.g., total antibody or free load) and the exposure levels across various organs. Tissue distribution studies can also be conducted using tumor model animals [2].
PD studies for ADCs can be divided into in vitro and in vivo studies. In vitro studies typically evaluate antigen affinity, Fc-mediated tumor killing (ADCC/ADCP), ADC internalization, payload mechanism of action, and bystander effects. In vivo PD studies generally use tumor animal models to assess the efficacy of ADCs, mainly employing mouse models such as cell line-derived xenografts (CDX) and patient-derived xenografts (PDX). CDX models offer consistent genetic and phenotypic traits, while PDX models more accurately reflect the heterogeneity and complexity of human tumors.
It is important to note that since both CDX and PDX models are based on immunodeficient mice, when it is necessary to consider immune system function (e.g., testing ADCs in combination with immune checkpoint inhibitors or when the payload is an immunomodulatory drug), humanized tumor models can be constructed using human peripheral blood mononuclear cells (PBMC) or hematopoietic stem cells (HSC), which can be used to evaluate the efficacy of immunomodulatory-related ADCs or their use in combination with immunotherapeutics[3].

Figure 2. Schematic diagram of the preclinical PK/PD study for ADC drugs, with asterisks (*) indicating studies of greater significance for ADCs with new linker/payload.
Increasingly, ADC research employs models that integrate PK, PD, and safety data[4] to meet the diverse needs throughout different stages of ADC development. Given that ADCs possess multiple clearance pathways and exhibit complex PK characteristics with various analytes, their PK models can be relatively intricate. Typically, two-compartment models or physiologically based pharmacokinetic (PBPK) models are used to calculate parameters such as clearance rates, dissociation, and metabolism rates, thereby analyzing the ADME characteristics of ADCs. Furthermore, combining pharmacodynamic data with PK/PD models can enhance the understanding of ADC pharmacology and potential safety risks in tumor models.
DS8201 in vivo PKPD validation
Shown below is an ADC drug validation experiment for a preclinical in vivo PKPD study of the DS8201 drug in HCC1954 and JMT-1 tumor-bearing mouse models. HCC1954 is an epithelial breast cancer cell line derived from a human primary stage IIA, grade 3 infiltrating ductal carcinoma, while JIMT-1 is a breast cancer cell line established from pleural effusion of a human ductal carcinoma. Both are commonly used tumor cell line models that express the HER2 antigen. Among them, HCC1954 has a higher HER2 expression level and is considered a high HER2 expression model.
The PK/PD validation study was designed with six groups, including high and low-dose experimental groups for DS8201 in the HCC1954 and JIMT-1 tumor models, along with control groups. Plasma samples were collected at nine time points post-administration, while tumor and tissue samples (from twelve different organs) were collected at four time points. The analyzed tissues included the brain, liver, spleen, lungs, heart, kidneys, stomach, small intestine, large intestine, muscle, ovaries, and uterus. The samples underwent bioanalysis for total antibody, conjugated antibody, and free payload.
In the experiment, immunodeficient mice were inoculated with cultured HCC1954 and JIMT-1 tumor cells. Once tumors reached approximately 200 mm³, a single intravenous (IV) dose of DS8201 was administered. Tumor volume was measured twice a week, serving as the primary pharmacodynamic endpoint. As illustrated, the tumor growth inhibition (TGI) rates in the HCC1954 model were 122.21% and 108.78% for high and low-dose groups, respectively (Figure 3), while in the JIMT-1 model, the rates were 81.56% and 63.2% (Figure 4). The HER2 high-expression model demonstrated a more pronounced response to DS8201, consistent with extensive clinical data on ADCs.

Figure 3. Relationship of tumor volume and treatment time for high and low dose DS8201 administration in the HC1954 tumor model, along with the calculation of tumor growth inhibition (TGI). In Figure 3A, the X-axis shows days post-administration, and the Y-axis represents tumor volume. In Figure 3B, the X-axis indicates days post-administration, while the Y-axis displays the percentage change in mouse body weight.

Figure 4. Relationship of tumor volume and treatment time for high and low dose DS8201 administration in the JIMT-1 tumor model, along with the calculation of tumor growth inhibition (TGI). In Figure 4A, the X-axis shows days post-administration, and the Y-axis represents tumor volume. In Figure 4B, the X-axis indicates days post-administration, while the Y-axis displays the percentage change in mouse body weight.
In the PKPD experiment, along with the investigation of the main pharmacodynamic indicators, we also investigated the pharmacokinetic characteristics of the total antibody, conjugated antibody, and free payload of DS8201 ADC drug in the systemic circulation and tumor tissues, as well as the tissue distribution of the primary tissues. The PK curves for total and conjugated antibodies in systemic circulation (plasma) and tumor tissues are shown in Figure 5, while the specific PK curves for free payload in systemic circulation and tumors are illustrated in Figure 6.
From the systemic circulation PK data, DS8201 exhibited good stability, with total antibody and conjugated antibody concentrations remaining relatively unchanged over a three-week sampling period. The free payload was only detectable early in the high-dose group, and a good linear relationship was observed between exposure and administered dose level of total antibody and conjugated antibody. However, tumor data indicated a nonlinear relationship between exposure and administered dose level of total antibody and conjugated antibody. This discrepancy is primarily due to the influence of target antigen expression and other factors on ADC distribution within tumors, indicating that ADC exposure and drug metabolism rates are closely linked to the tumor model itself.
Additionally, a positive correlation was found between the exposure level of total antibody and conjugated antibody and the antigen expression level in tumors. In models with high antigen expression, total antibody, and conjugated antibody exposure levels were 1.5 times higher than those in low expression models. The difference in free payload exposure level between high and low antigen expression models was even more pronounced. Tumor cells with high antigen expression facilitate ADC internalization and payload release, aligning with previous research findings. When combined with PD outcomes showing tumor growth inhibition, higher exposure levels of total antibody, conjugated antibody, and free payload correlated positively with TGI.

Figure 5. PK curves of total and conjugated antibodies for high and low doses of DS8201 in HCC1954 and JIMT-1 tumor models. Figure 5A shows the relationship between total and conjugated antibody concentrations over time in the tumor tissue of the HCC1954 model, with the X-axis representing days post-administration and the Y-axis indicating drug concentration in tumor tissue (µg/g). Refer to Figure 5B for the corresponding plasma concentrations in the HCC1954 model, where the X-axis is days post-administration, and the Y-axis is drug concentration in plasma (µg/mL). Figure 5C presents the concentration-time relationship of total and conjugated antibodies in the tumor tissue of the JIMT-1 model, with the same axes as in Figure 5A. Figure 5D illustrates the plasma concentrations for the JIMT-1 model, with the same axes as in Figure 5B.

Figure 6. PK curves of free payload for different doses of DS8201 in HCC1954 and JIMT-1 tumor models. Figure 6A depicts the concentration-time relationship of free payload in the tumor tissue of the HCC1954 model, with the X-axis showing days post-administration and the Y-axis indicating drug concentration in tumor tissue (ng/g). Figure 6B shows the plasma concentrations in the HCC1954 model, with the X-axis as days post-administration and the Y-axis as drug concentration in plasma (ng/mL). Figure 6C presents the free payload concentration-time relationship in the tumor tissue of the JIMT-1 model, with the same axes as in Figure 6A. Figure 6D illustrates the plasma concentrations in the JIMT-1 model, with the same axes as in Figure 6B.
These observations and conclusions align with existing literature on ADC research [5][6], further validating the relationship between payload exposure within tumors and therapeutic efficacy [7]. We also assessed the tissue distribution of DS8201 using an efficacy tumor model, which provides a more accurate representation of drug distribution than healthy animal models, as recommended by regulatory guidelines for ADC tissue distribution studies [8].
The tissue distribution data showed that ADC was mainly distributed in tumor tissues, with minor distributions in the uterus, lungs, kidneys, and liver, while the free payload was only detected in small intestinal tissues and not in other tissues. The exposure levels of high and low-dose DS8201 across various tissues in the HCC1954 and JIMT-1 tumor models are illustrated in Figure 7. The data indicates that non-target tissue exposure in high antigen expression models is generally lower than in low antigen expression models, suggesting that ADC distribution in non-target tissues is influenced by its distribution in target tissues. This highlights potential differences in tissue distribution between normal and tumor-bearing animal models.

Figure 7. Tissue exposure distribution of different doses of DS8201 in HCC1954 and JIMT-1 tumor models. Figures 7A and 7B show the tissue exposure levels of the ADC drug in the low and high-dose groups of the JIMT-1 tumor model, with the X-axis representing different tissues and the Y-axis indicating exposure (AUC0-last ng·h/mL). Figures 7C and 7D depict the tissue exposure levels of the ADC drug in the low and high-dose groups of the HCC1954 tumor model, with the same axes as in Figures 7A and 7B.
Summary: The PK/PD validation experiments of DS8201 demonstrate a strong correlation between the release of the payload in target tissues (tumor tissue concentration of payload) and tumor efficacy (TGI). In light of reported preclinical and clinical data for ADCs, we recommend focusing on in vitro ADC internalization studies, in vitro stability studies, and in vivo PK/PD studies during the early research phases of ADC development. For novel payloads and linkers, it is also essential to investigate ADC payload release in target and non-target tissues, bystander effects, in vitro ADME studies of payloads or major metabolites (especially efflux transporters), in vivo ADME studies, and identification studies of major metabolites (met ID) both in vitro and in vivo.
The bottom line
In the early stages of drug discovery, the efficacy of ADCs is a primary focus. However, understanding the pharmacokinetic characteristics is equally important. It is essential to evaluate the stability of ADC candidates and their biotransformation processes, which includes understanding how the payload is released from the antibody while effectively killing cancer cells without reaching harmful systemic exposure levels. DMPK studies can clarify the relationship between the efficacy and potential toxicity of ADCs, aiding developers in selecting appropriate linkers and payloads and in designing the antibody component more effectively. Research on the absorption, distribution, metabolism, and excretion (ADME) characteristics of candidate ADCs, combined with in vivo PK analysis data, will ultimately determine the potential of these drugs as effective therapies.
DMPK and Biology teams at WuXi AppTec have extensive experience in preclinical ADC development, having conducted over 100 ADC pharmacokinetic and pharmacodynamic study projects, including several IND submissions. We can assist clients in efficiently completing early ADC discovery and preclinical IND application work, rapidly optimizing and screening ADC candidates through in vitro and in vivo efficacy and pharmacokinetic platforms, and laying a solid foundation for subsequent safety evaluations and clinical studies.
Authors: Xue Zhang, Maotian Zhou, Lili Xing
Talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,600+ global clients, and have successfully supported 1,500+ IND applications.
Reference
[1] Hedrich, William D., et al. "Antibody–drug conjugates: pharmacokinetic/Pharmacodynamic modeling, preclinical characterization, clinical studies, and lessons learned." Clinical pharmacokinetics 57 (2018): 687-703.
[2] Beaumont, Kevin, et al. "ADME and DMPK considerations for the discovery and development of antibody drug conjugates (ADCs)." Xenobiotica 52.8 (2022): 770-785.
[3] Yin, Ling, et al. "Humanized mouse model: a review on preclinical applications for cancer immunotherapy." American Journal of Cancer Research 10.12 (2020): 4568.
[4] Lam, Inez, et al. "Development of and insights from systems pharmacology models of antibody‐drug conjugates." CPT: Pharmacometrics & Systems Pharmacology 11.8 (2022): 967-990.
[5] Okamoto, Hiromi, et al. "Pharmacokinetics of trastuzumab deruxtecan (T-DXd), a novel anti-HER2 antibody-drug conjugate, in HER2-positive tumour-bearing mice." Xenobiotica 50.10 (2020): 1242-1250.
[6] Nagai, Yoko, et al. "Comprehensive preclinical pharmacokinetic evaluations of trastuzumab deruxtecan (DS-8201a), a HER2-targeting antibody-drug conjugate, in cynomolgus monkeys." Xenobiotica 49.9 (2019): 1086-1096.
[7] Zhang, Donglu, et al. "Exposure-efficacy analysis of antibody-drug conjugates delivering an excessive level of payload to tissues." Drug Metabolism and Disposition 47.10 (2019): 1146-1155.
[8] Technical Guidelines for Non-clinical Research of Antibody-Drug Conjugates, Center for Drug Evaluation, NMPA
Related Services and Platforms




-

 DMPK BioanalysisLearn More
DMPK BioanalysisLearn More -

 Novel Drug Modalities DMPK Enabling PlatformsLearn More
Novel Drug Modalities DMPK Enabling PlatformsLearn More -

 Novel Drug Modalities BioanalysisLearn More
Novel Drug Modalities BioanalysisLearn More -

 Small Molecules BioanalysisLearn More
Small Molecules BioanalysisLearn More -

 Bioanalytical Instrument PlatformLearn More
Bioanalytical Instrument PlatformLearn More -

 PROTAC DMPK ServicesLearn More
PROTAC DMPK ServicesLearn More -

 ADC DMPK ServicesLearn More
ADC DMPK ServicesLearn More -

 Oligo DMPK ServicesLearn More
Oligo DMPK ServicesLearn More -

 PDC DMPK ServicesLearn More
PDC DMPK ServicesLearn More -

 Peptide DMPK ServicesLearn More
Peptide DMPK ServicesLearn More -

 mRNA DMPK ServicesLearn More
mRNA DMPK ServicesLearn More -

 Covalent Drugs DMPK ServicesLearn More
Covalent Drugs DMPK ServicesLearn More
Stay Connected
Keep up with the latest news and insights.