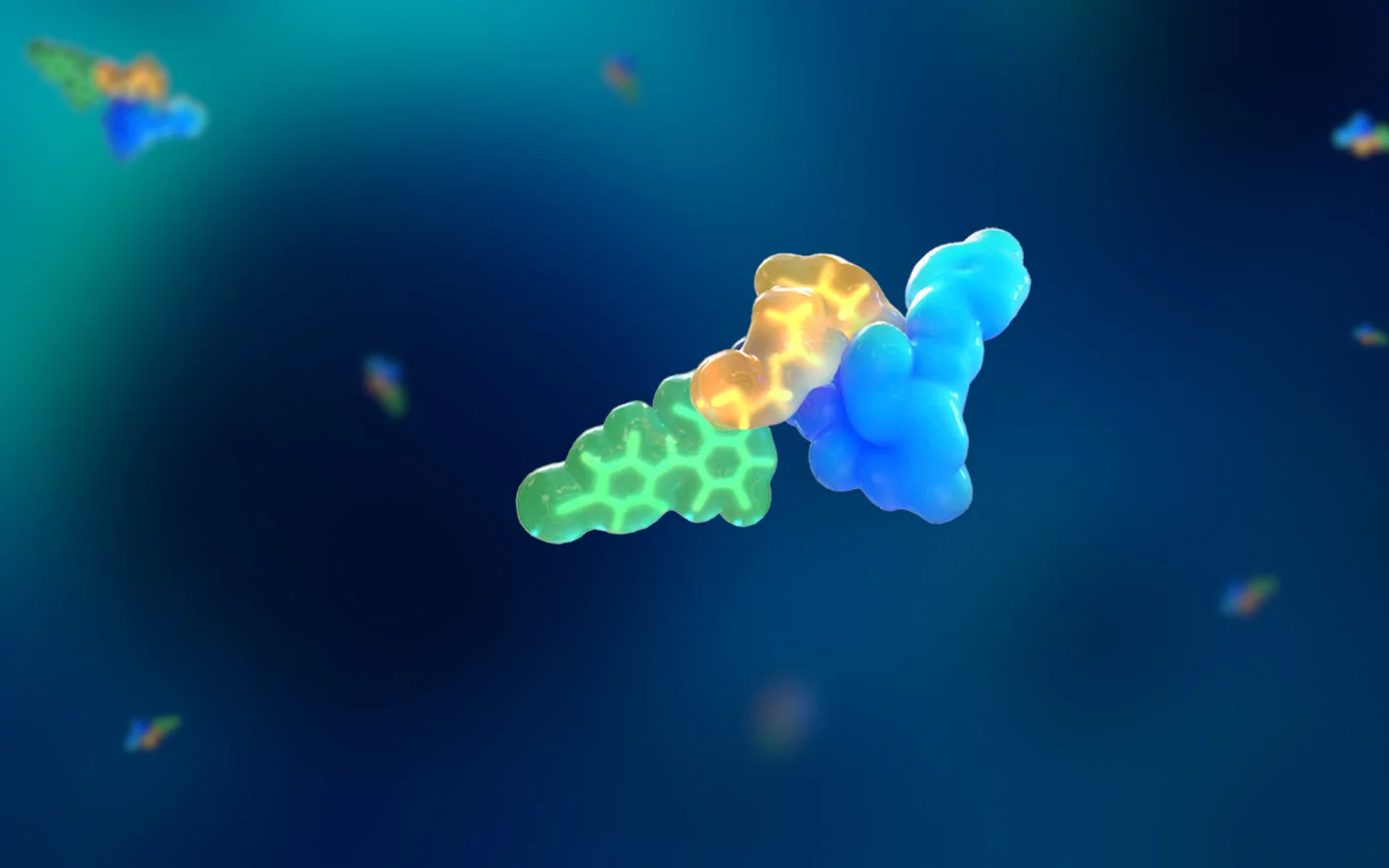
Chemotherapy plays a crucial role in cancer treatment. Chemotherapeutic agents have been developed based on different mechanisms that can target initial materials such as purines and pyrimidines required for nucleotide synthesis, as well as deoxynucleotides for DNA replication or ribonucleotides required for RNA transcription, or directly on DNA, RNA, and proteins of the central dogma of molecular biology. As an important component of the cytoskeleton, tubulin is involved in many cellular processes that are essential for cell function, such as cell migration and mitosis. As a classic anticancer drug, paclitaxel acts as a tubulin stabilizer, while vinblastine acts as a destabilizer of tubulin.

Figure 1. Mechanism of action of commonly used chemotherapy drugs
To improve the targeting of chemotherapy drugs, researchers have conducted preclinical and clinical studies since the late 1950s on conjugates made from murine antibodies and various chemotherapy agents like doxorubicin and methotrexate, significantly advancing ADC development[1]. ADCs can be seen as an evolution of chemotherapy drugs. However, the initial “first-generation ADCs” failed largely due to poor targeting and insufficient potency, leading to limited efficacy and retained toxicity. While some highly toxic compounds are unsuitable for standalone use as drugs, they may serve effectively as payloads for ADCs. As ADCs achieve clinical success, their combination with immune checkpoint inhibitors is increasingly likely to replace traditional chemotherapy and immune checkpoint inhibitor combinations [2]. ADCs are poised to surpass chemotherapy drugs in the future.
Highly potent cytotoxic drugs
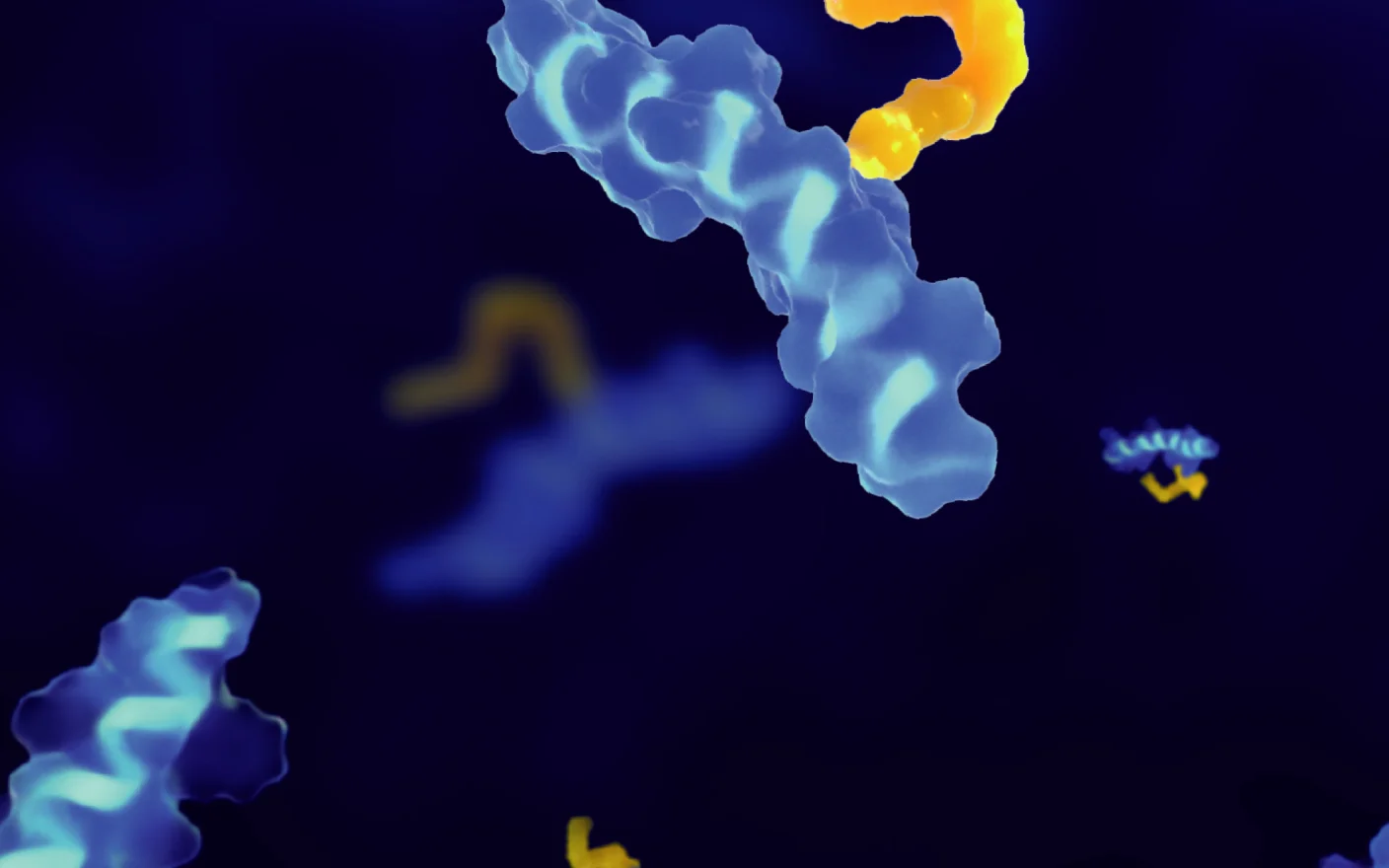
Currently approved ADC payloads, such as MMAE/MMAF, carchimycin, DM1/DM4, and SN38/Dxd, exhibit significantly higher toxicity—up to 1-2 orders of magnitude greater than traditional chemotherapy drugs, with some reaching picomolar levels (see Figure 2)[3]. The mechanism of action of currently developed payloads is primarily limited to DNA alkylating agents, DNA topoisomerase inhibitors, tubulin disruptors, and RNApolII inhibitors.
|
Target |
Mechanism of action |
Payload |
Bystander effect |
Major toxicity caused by the payload |
Representative examples on the market or in the clinical stage |
|
|
DNA |
DNA alkylating agent |
Carchimycin |
Yes |
Bone marrow suppression, elevated liver enzymes, etc |
Besponsa |
|
|
Duocarmycins |
Yes |
ocular toxicity, fatigue, and interstitial pneumonia (ILD), etc. |
SYD985 |
|||
|
Apertoxin-like PBD, etc |
Yes |
Hematotoxicity, phototoxicity |
Zynlonta |
|||
|
Topoisomerase I inhibitors (TOPO1) |
Camptothecin and SN38 |
Yes |
Gastrointestinal toxicity and hematotoxicity |
Trodelvy |
||
|
Exatecan and its derivatives |
Yes |
Diarrhea, neutropenia, and thrombocytopenia |
AZD8205 |
|||
|
Dxd |
Yes |
Similar to Exatecan, but bone marrow toxicity of Dxd is lower |
Enhertu |
|||
|
Topoisomerase II inhibitor (TOPO2) |
PNU-159682 |
Unknown |
Unknown |
CD22-NMS249 ADC |
||
|
RNA |
RNApolII inhibitors |
α-Amanita amanitamine |
No |
Hepatotoxicity |
HDP-101 |
|
|
Tubulin |
Microtubule destabilizer |
Nudibranchs toxin |
MMAE |
Yes |
Anemia, neutropenia, and peripheral neuropathy |
Padcev |
|
MMAF |
No |
Ocular toxicity and pulmonary toxicity |
Blenrep |
|||
|
Maytanol |
DM1 |
Yes* |
Thrombocytopenia, hepatotoxicity |
Kadcyla |
||
|
DM4 |
Yes |
Ocular toxicity, hepatotoxicity |
Elahere |
|||
|
Tubulysins |
Unknown |
Hepatotoxicity |
MEDI4276 |
|||
|
Binds to β-tubulin and inhibits the elongation of microtubules |
Soft spondrocins: eribulin |
Yes |
Interstitial pneumonia (ILD) |
MORAb-202 |
||
Table 1. Mechanism of action, bystander effect, and associated toxicities of payload, and representative examples
* Permeability of DM1 is not bad. DM1 is connected to a non-cleavable linker in Kadcyla, and the released DM1 is connected to a partial linker with a negative charge, and the permeability deteriorates, resulting in no bystander effect in Kadcyla.
Table 1 summarizes the mechanism of action of ADC payloads, the bystander effect, and the associated toxicity caused by the payload [4]. However, the availability of highly potent cytotoxic drugs is limited, creating an urgent need to develop new cytotoxic agents with high potency and diverse mechanisms of action. While there have been many introductions to the payloads of marketed ADCs [5], this article will provide a brief introduction to the newly developed non-traditional payloads not yet used in the marketed ADCs, including dukamycin, PNU-159682, Amanitin, Tubulysins, and eribulin.

Figure 2. IC50 range of common cytotoxic drugs [3].
Duramycin
Dukamycin is a DNA alkylating agent that can act on the full cycle of tumor cells with in vitro activity at the picomolar level. Ducamycin has good permeability and a "bystander effect", and it remains active against cell lines with multidrug-resistant (MDR) efflux transporters.
SYD985 is a HER2-targeting ADC developed by Byondis [6]. In SYD985, tratuzumab is linked to ducamycin through a cleavable linker with a DAR value of 2.8. After cleavage by cathepsin B, released free phenol promotes intramolecular rearrangement into an electrophilic cyclopropyl form, which easily forms a covalent bond with DNA, resulting in DNA alkylation. Major safety concerns with SYD985 include ocular toxicity and interstitial pneumonia (ILD).

Figure 3. Structure of SYD 985 and schematic diagram of DUBA released by in vivo proteolysis.
PNU-159682
Osteosarcoma is the most common malignant bone tumor in children and adolescents, and it can recur or metastasize remotely after surgery in about 40~50% of patients, resulting in a 5-year survival rate of less than 30%. Anthracyclines, including doxorubicin, are first-line chemotherapy agents for osteosarcoma, affecting DNA replication and RNA synthesis through DNA intercalation. As an ADC payload, adriamycin lacks sufficient cytotoxicity (IC50 shown in Figure 2), prompting the development of PNU-159682, which exhibits 100 times greater cytotoxicity. PNU-159682, a liver metabolite of nemorubicin, inhibits DNA topoisomerase II and is three orders of magnitude more potent, with an IC50 of 20-100 picomolar. Additionally, PNU-159682 is not a substrate of the efflux transporter [5d].

Figure 4. Nemorubicin is converted to PNU-159682 in the liver.
Genentech has developed a novel anti-CD22-NMS249 ADC based on PNU-159682 using the MC-VC-PAB-DEA linker with a DAR value of 2 (Figure 5). The anti-CD22-NMS249 ADC demonstrates at least equal efficacy to the anti-CD22-VC-MMAE ADC in xenograft tumor models and remains effective against cell lines resistant to CD22-VC-MMAE ADCs[4]. No toxicity related to PNU-159682 has been reported in clinical trials to date.

Figure 5. Structure of the anti-CD22-NMS249 ADC.
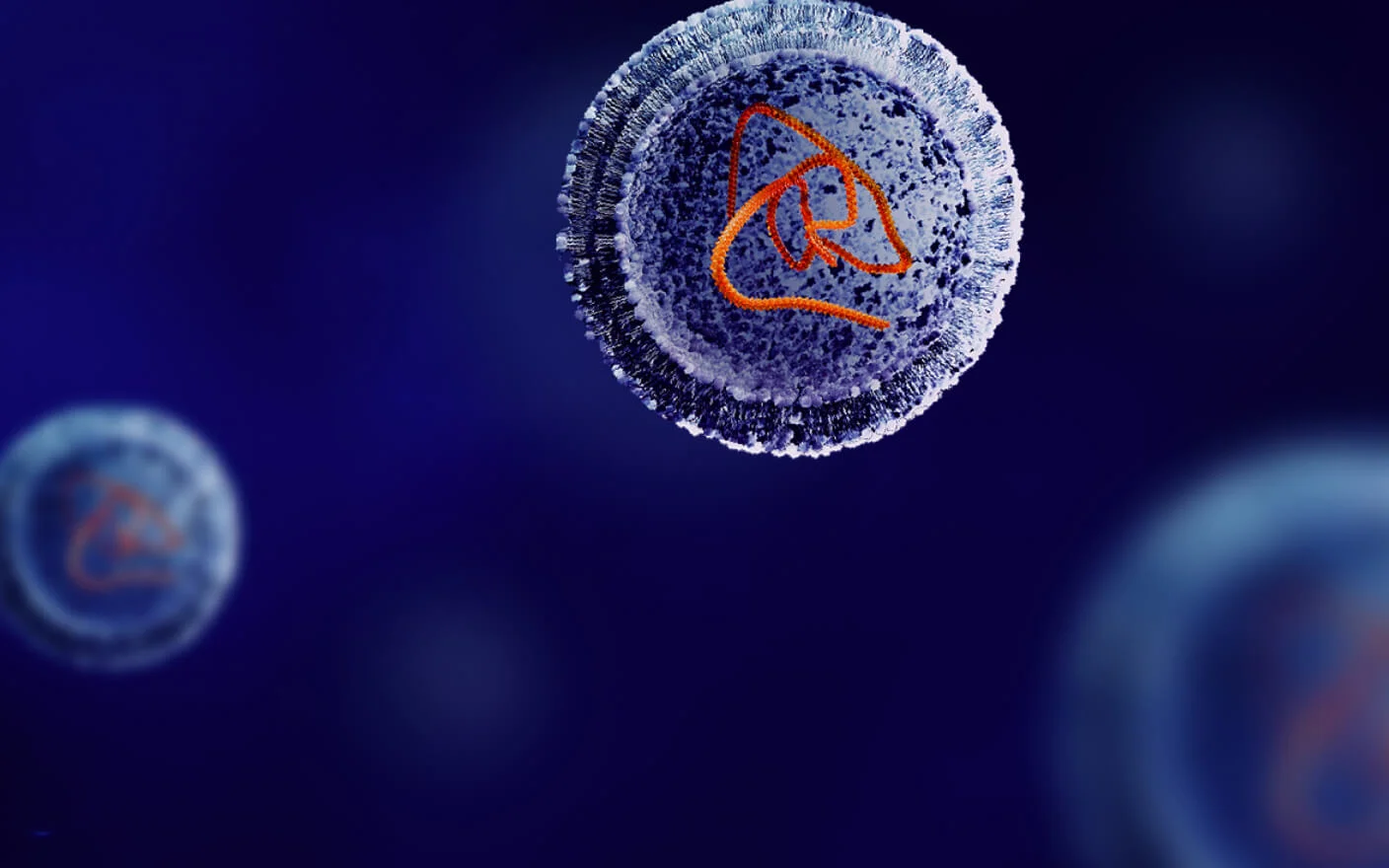
Amanitin
The amanitin family is composed of nine structurally similar toxins, derived from the world's most virulent mushroom. Among these, α-amanitin and β-amanitin are the most significant, being bicyclic peptides made up of eight amino acids. Ingestion of Amanita phalloides causes vomiting, seizures, and severe liver damage (amanitin is a substrate for liver transporter OATP1B3), which is responsible for 90% of mushroom-related deaths. Amanitin is a highly potent RNApolII inhibitor with cytotoxicity at the picomolar level, which can efficiently bind to RNA polymerase II in eukaryotes, thereby reducing RNA transcription and protein synthesis efficiency by more than 1000 times. Therefore, amanitin can kill not only tumor cells in the division stage, but also cells in the dormant stage, including cancer stem cells. While too toxic for standalone use as an anticancer agent, amanitin offers several advantages as an ADC payload, including high toxicity, hydrophilicity, and being a non-P-glycoprotein (P-gp) substrate.
HDP-101 is an ADC developed by Heidelberg Pharma targeting BCMA and consists of a BCMA antibody, a VA-PABC linker, and an Amanitin derivative, HDP 30.2115. Given its high toxicity, HDP-101 has a DAR of 2, employing site-specific conjugation to ensure uniformity and minimize potential toxicity [7]. In May 2021, HDP-101 entered an early-phase clinical trial for the treatment of multiple myeloma (NCT04879043). Recent findings indicate that HDP-101 can activate the immune system, induce immunogenic cell death (ICD), and exhibit synergistic effects with immune checkpoint inhibitors, paving the way for potential combination therapies.

Figure 6. α-amanitin and β-amanitin and HDP-101 structures
Tubulysins
Tubulysin natural products are toxic tetrapeptides isolated from myxobacteria species that inhibit microtubule polymerization. The cytotoxicity of these natural products is 10-1000 times higher than that of vinblastine and paclitaxel (IC50 in the picomolar level), and the cells are impeded in the G2/M phase by inhibiting microtubule polymerization. And tubulysin is not a substrate of multidrug resistance efflux transporters. Researchers are exploring the structure-activity relationship (SAR) of tubulysin-like natural products, aiming to develop these molecules as new ADC payloads.

Figure 7. Tubulysins family and MEDI4276 structure
AstraZeneca/MedImmune has developed the bispecific ADC MEDI4276[8], which targets two distinct HER2 epitopes. This bispecificity may enhance internalization, increasing payload release and improving cancer cell lethality. MEDI4276 consists of a bispecific antibody linked to the tubulysin derivative AZ13599185 by a non-cleavable linker with a DAR value of 4. MEDI4276 has demonstrated promising anti-tumor activity in preclinical studies, with hepatotoxicity being the primary concern in clinical trials.
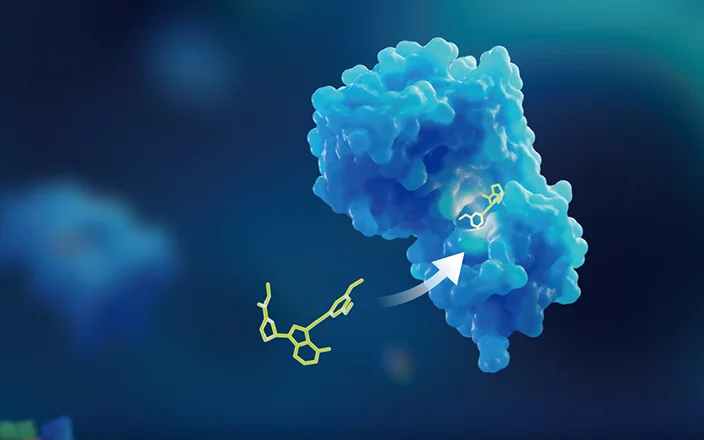
Eribulin
Eribulin is a synthetic analogue of halichondrin B, derived from sponges. Eribulin selectively binds to the β-tubulin (+) terminus, inhibiting microtubule elongation while minimally affecting depolymerization, making it effective in paclitaxel-resistant patients. In November 2010, eribulin was approved by the FDA for the treatment of metastatic breast cancer. As an ADC payload, eribulin exhibits a strong “bystander effect,” contributing to its clinical efficacy. In addition, eribulin is less sensitive to P-glycoprotein (P-gp) efflux transporters.
MORAb-202, an ADC developed by Eisai targeting FRα, uses eribulin as a payload (Figure 8). The antibody is farletuzumab, a humanized monoclonal antibody against the folate receptor α, which connects to eribulin by an enzymatically cleavable linker with a DAR value of 4. Mirvetuximab soravtansine, developed by ImmunoGen, has the fastest progress among ADC targeting FRα, which had an overall response rate (ORR) of 22% in the Phase III trial (FORWARD I, n=336), while MORAb-202 achieved an ORR of 45.5% in the Phase I clinical trial (NCT03386942, n=22) and it was well tolerated, exhibiting best-in-class potential. The primary associated toxicity related to MORAb-202 was grade 1/2 interstitial pneumonia.

Figure 8. MORAb-202 structure
In vitro and in vivo pharmacokinetic studies of ADC payloads
Based on the Guidelines for Non-clinical Research of Antibody-Drug Conjugates by NMPA and the research experience from WuXi AppTec DMPK, it is recommended to conduct relevant in vitro and in vivo pharmacokinetic studies for new payloads.
-
Plasma protein binding (PPB): The payload concentration in the plasma after ADC administration is generally low, so PPB should be carried out at a low concentration of payload to mimic in vivo conditions. However, due to the sensitivity limitation of the detection method, when the payload cannot be detected by conventional mass spectrometry, radiolabeled payloads can be used to carry out PPB assay.
-
Tissue distribution and excretion/mass balance: Similarly, due to the sensitivity limitation of the detection method, it is challenging to study tissue distribution and excretion by using conventional mass spectrometry. Achieving a high excretion recovery rate with non-radiolabeled payloads is difficult, making it challenging to determine the excretion pathway and whether highly toxic payloads can be effectively eliminated from the body. Consequently, radiolabeled payloads are often recommended for studying the ADME characteristics of the payload in vivo. For tissue distribution studies, quantitative whole-body autoradiography (QWBA) is recommended, as it offers a detailed view of payload distribution across tissues, particularly in areas like skin and eyes that are challenging to assess through tissue removal.
-
In vitro and in vivo metabolism studies: To ensure metabolic stability, the ideal payload must be rapidly metabolized upon entering the circulatory system to minimize systemic exposure and toxicity. Understanding potential species differences in payload metabolism is essential, and the selection of toxicological animal models should consider this to identify human-related species. Additionally, plasma collected during toxicokinetic (TK) assays should be used for identifying payload-related metabolites, comparing these results with human plasma data after ADC administration to assess whether metabolite exposure in toxicological species is representative of humans.
-
Effect on metabolic enzymes: This evaluation includes whether the payload inhibits or induces drug-metabolizing enzymes, and the identification of the subtypes of drug-metabolizing enzymes involved in payload metabolism. Theoretically, the payload has a low blood concentration in vivo, and the risk as an inhibitor or inducer of metabolic enzymes is low. Similarly, due to the low plasma concentration of the payload, if the payload is known to be a substrate of a metabolic enzyme, inhibition of the enzyme may significantly increase the plasma concentration of the payload in vivo, thereby increasing toxicity. Therefore, in the preclinical stage, a phenotyping study to figure out the payload metabolic enzyme is essential.
-
Effect on transporters: The evaluation includes whether the payload is a transporter substrate or a transporter inhibitor. Since the concentration of payload is generally low in vivo, the risk of payload acting as a transporter inhibitor is theoretically low. The uptake or efflux of transporters affects the distribution or excretion of drugs in vivo. If the payload is the substrate of uptake or efflux transporter, it can affect the distribution of the payload in certain transporter-expressing tissues, increasing the risk of toxicity to the tissues. Tumor tissues generally overexpress efflux transporters, such as P-gp, BCRP, or MRPs. If the payload is a substrate of P-gp, BCRP, or MRPs, the effect of the efflux transporter will reduce the accumulation of payload in the tumor tissue, which will ultimately affect the efficacy and drug resistance.
-
PK/PD studies: Although the antibody of ADC may interact with immune effector cells, including CDC (complement-dependent cytotoxicity), ADCC (antibody-dependent cytotoxicity), and ADCP (antibody-dependent cellular phagocytosis) effects, the efficacy of the ADC primarily derives from the payload. Zhang et al. [9, 10] compared the efficacy of different ADCs with PBD as a payload on tumor mice, where the anti-tumor effect was directly related to the exposure of the intratumoral payload. Additionally, as the target (DNA) becomes saturated over time, the anti-tumor effect tends to stabilize. A similar phenomenon was observed in the tumor-bearing mice model with MMAE as a payload. This study indicates that the anti-tumor efficacy of ADCs is not linked to systemic ADC exposure or plasma payload exposure but is directly associated with payload exposure within the tumor. Considering this, it is necessary to carry out PK studies in the tumor by using model animals to evaluate the PK/PD of ADCs.

Figure 9. Relationship between drug concentration and tumor inhibition in tumor tissues in animal models[9].
Summary and perspective
Desirable payload properties for an ADC include:
-
A unique mechanism of action distinct from commonly used chemotherapy drugs to effectively circumvent cross-drug resistance;
-
Strong potency with IC50 at picomolar level;
-
Suitable site to connect with the linker;
-
Aqueous solubility to facilitate coupling with the antibody;
-
Rapid elimination in the blood circulatory system to reduce system toxicity;
-
Be substrates of non-efflux transporters to avoid drug resistance;
-
A “bystander effect” to target heterogeneous tumors.
This article introduces newly developed non-traditional payloads that have not yet been utilized in marketed ADCs. For the development of payloads, in addition to the continuous screening, optimization, and improvement of various types of cytotoxins, there are also dual payloads, [11a], as well as payloads with different mechanisms of action, such as nuclides, glucocorticoids [11b], PROTAC [11c], and RNA, etc. The applications of ADCs have broadened beyond tumors to encompass various disease areas, including infections and autoimmune disorders.
Authors: Qigan Cheng, Liping Ma, Jing Jin
Talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,600+ global clients, and have successfully supported 1,500+ IND applications.
Reference
[1]Goldenberg DM, Sharkey RM. Sacituzumab govitecan, is a novel, third-generation, antibody-drug conjugate (ADC) for cancer therapy. Expert Opin Biol Ther. 2020 Aug; 20(8):871-885. doi: 10.1080/14712598.2020.1757067. Epub 2020 May 12. PMID: 32301634.
[2]Fuentes-Antrás J, Genta S, Vijenthira A, Siu LL. Antibody-drug conjugates: in search of partners of choice. Trends Cancer. 2023 Apr; 9(4):339-354. doi: 10.1016/j.trecan.2023.01.003. Epub 2023 Feb 4. PMID: 36746689.
[3]Nakada T, Sugihara K, Jikoh T, Abe Y, Agatsuma T. The Latest Research and Development into the Antibody-Drug Conjugate, [fam-] Trastuzumab Deruxtecan (DS-8201a), for HER2 Cancer Therapy. Chem Pharm Bull (Tokyo). 2019; 67(3):173-185. doi: 10.1248/cpb.c18-00744. PMID: 30827997.
[4]Related literature on payload toxicity: (a)Hinrichs MJ, Dixit R. Antibody Drug Conjugates: Nonclinical Safety Considerations. AAPS J. 2015; 17(5):1055-1064. doi:10.1208/s12248-015-9790-0; (b) Fisher JE Jr. Considerations for the Nonclinical Safety Evaluation of Antibody-Drug Conjugates. Antibodies (Basel). 2021 Apr 19; 10(2):15. doi: 10.3390/antib10020015. PMID: 33921632; PMCID: PMC8167597; (c) Masters JC, Nickens DJ, Xuan D, et al. Clinical toxicity of antibody drug conjugates: a meta-analysis of payloads. Invest New Drugs. 2018 Feb; 36(1):121-135. (d)Cortés J, Kim SB, Chung WP, Im SA, Park YH, Hegg R, Kim MH, Tseng LM, Petry V, Chung CF, Iwata H, Hamilton E, Curigliano G, Xu B, Huang CS, Kim JH, Chiu JWY, Pedrini JL, Lee C, Liu Y, Cathcart J, Bako E, Verma S, Hurvitz SA; DESTINY-Breast03 Trial Investigators. Trastuzumab Deruxtecan versus Trastuzumab Emtansine for Breast Cancer. N Engl J Med. 2022 Mar 24; 386(12):1143-1154. doi: 10.1056/NEJMoa2115022. PMID: 35320644.
[5](a)Cytotoxic payloads for Antibody – Drug Conjugates, Hardback ISBN: 978-1-78801-077-1PDF ISBN: 978-1-78801-289-8EPUB ISBN: 978-1-78801-845-6. Publication date: 11 Jul 2019. DOI: http://doi.org/10.1039/9781788012898. (b) Cheng-Sánchez I, Moya-Utrera F, Porras-Alcalá C, López-Romero JM, Sarabia F. Antibody-Drug Conjugates Containing Payloads from Marine Origin. Mar Drugs. 2022 Jul 30; 20(8):494. doi: 10.3390/md20080494. PMID: 36005497; PMCID: PMC9410405. (c)胡馨月,李艳萍,李卓荣,抗体药物偶联物的弹头分子研究进展,中国医药生物技术,2017, 012(006): 549-555. (d)Conilh L, Sadilkova L, Viricel W, Dumontet C. Payload diversification: a key step in the development of antibody-drug conjugates. J Hematol Oncol. 2023 Jan 17; 16(1):3. doi: 10.1186/s13045-022-01397-y. PMID: 36650546; PMCID: PMC9847035.
[6]Joubert N, Beck A, Dumontet C, Denevault-Sabourin C. Antibody-Drug Conjugates: The Last Decade. Pharmaceuticals (Basel). 2020 Sep 14; 13(9):245. doi: 10.3390/ph13090245. PMID: 32937862; PMCID: PMC7558467.
[7]Pahl A, Lutz C, Hechler T. Amanitins and their development as a payload for antibody-drug conjugates. Drug Discov Today Technol. 2018 Dec;30:85-89. doi: 10.1016/j.ddtec.2018.08.005. Epub 2018 Sep 24. PMID: 30553524.
[8]Li JY, Perry SR, Muniz-Medina V, Wang X, Wetzel LK, Rebelatto MC, Hinrichs MJ, Bezabeh BZ, Fleming RL, Dimasi N, Feng H, Toader D, Yuan AQ, Xu L, Lin J, Gao C, Wu H, Dixit R, Osbourn JK, Coats SR. A Biparatopic HER2-Targeting Antibody-Drug Conjugate Induces Tumor Regression in Primary Models Refractory to or Ineligible for HER2-Targeted Therapy. Cancer Cell. 2016 Jan 11; 29(1):117-29. doi: 10.1016/j.ccell.2015.12.008. Erratum in: Cancer Cell. 2019 Jun 10; 35(6):948-949. PMID: 26766593.
[9]Su D, Zhang D. Linker Design Impacts Antibody-Drug Conjugate Pharmacokinetics and Efficacy via Modulating the Stability and Payload Release Efficiency. Front Pharmacol. 2021 Jun 23;12:687926. doi: 10.3389/fphar.2021.687926. PMID: 34248637; PMCID: PMC8262647.
[10]Zhang D, Yu SF, Khojasteh SC, Ma Y, Pillow TH, Sadowsky JD, Su D, Kozak KR, Xu K, Polson AG, Dragovich PS, Hop CECA. Intratumoral Payload Concentration Correlates with the Activity of Antibody-Drug Conjugates. Mol Cancer Ther. 2018 Mar; 17(3):677-685. doi: 10.1158/1535-7163.MCT-17-0697. Epub 2018 Jan 18. PMID: 29348271.
[11](a)Nilchan N, Li X, Pedzisa L, Nanna AR, Roush WR, Rader C. Dual-mechanistic antibody-drug conjugate via site-specific selenocysteine/cysteine conjugation. Antib Ther. 2019 Oct; 2(4):71-78. doi: 10.1093/abt/tbz009. Epub 2019 Oct 24. PMID: 31930187; PMCID: PMC6953743. (b)Dragovich PS. Antibody-Drug Conjugates for Immunology. J Med Chem. 2022 Mar 24; 65(6):4496-4499. doi: 10.1021/acs.jmedchem.2c00339. Epub 2022 Mar 14. PMID: 35285623. (c)Pillow TH, Adhikari P, Blake RA, Chen J, Del Rosario G, Deshmukh G, Figueroa I, Gascoigne KE, Kamath AV, Kaufman S, Kleinheinz T, Kozak KR, Latifi B, Leipold DD, Sing Li C, Li R, Mulvihill MM, O'Donohue A, Rowntree RK, Sadowsky JD, Wai J, Wang X, Wu C, Xu Z, Yao H, Yu SF, Zhang D, Zang R, Zhang H, Zhou H, Zhu X, Dragovich PS. Antibody Conjugation of a Chimeric BET Degrader Enables in vivo Activity. ChemMedChem. 2020 Jan 7; 15(1):17-25. doi: 10.1002/cmdc.201900497. Epub 2019 Nov 14. PMID: 31674143.
Related Services and Platforms




-

 In Vitro ADME ServicesLearn More
In Vitro ADME ServicesLearn More -

 Novel Drug Modalities DMPK Enabling PlatformsLearn More
Novel Drug Modalities DMPK Enabling PlatformsLearn More -

 Physicochemical Property StudyLearn More
Physicochemical Property StudyLearn More -

 Permeability and Transporter StudyLearn More
Permeability and Transporter StudyLearn More -

 Drug Distribution and Protein Binding StudiesLearn More
Drug Distribution and Protein Binding StudiesLearn More -

 Metabolic Stability StudyLearn More
Metabolic Stability StudyLearn More -

 Drug Interactions StudyLearn More
Drug Interactions StudyLearn More -

 PROTAC DMPK ServicesLearn More
PROTAC DMPK ServicesLearn More -

 ADC DMPK ServicesLearn More
ADC DMPK ServicesLearn More -

 Oligo DMPK ServicesLearn More
Oligo DMPK ServicesLearn More -

 PDC DMPK ServicesLearn More
PDC DMPK ServicesLearn More -

 Peptide DMPK ServicesLearn More
Peptide DMPK ServicesLearn More -

 mRNA DMPK ServicesLearn More
mRNA DMPK ServicesLearn More -

 Covalent Drugs DMPK ServicesLearn More
Covalent Drugs DMPK ServicesLearn More
Stay Connected
Keep up with the latest news and insights.