This article provides a comprehensive overview of approved small interfering RNA (siRNA) drugs since 2008. It presents a summary of in vivo and in vitro pharmacokinetic (PK) studies based on application materials for these marketed siRNA drugs. The study designs and data characteristics of five approved drugs are analyzed in terms of absorption, distribution, metabolism, excretion (ADME), and Drug-Drug Interaction (DDI). These insights serve as a valuable reference for future investigations of candidate siRNA drugs.
All five marketed siRNA drugs are designed to target the liver, focusing on treating liver-related diseases. The pioneer drug, Patisiran, received approval in 2018. Patisiran utilizes a lipid nanoparticle (LNP) formulation containing two partially complementary single-stranded siRNAs and four lipid excipients. The encapsulation within LNPs safeguards the siRNAs from endogenous nucleases and facilitates targeted delivery to the liver. Subsequent siRNA drugs introduced between 2019 and 2022 employ a modified delivery system incorporating N-Acetyl-D-galactosamine (GalNAc). Intravenous (IV) infusion is generally used for LNP-targeted siRNAs, while GalNAc-modified delivery systems are administered via subcutaneous (SC) injection (Table 1).
First Approval Year | Drug name | Company | Drug type | Target | Indication | Route of administration |
2018 | Patisiran | Alnylam | siRNA | TTR | Hereditary TTR amyloidosis | IV |
2019 | Givosiran | Alnylam | siRNA | ALAS1 | Acute hepatic porphyria | SC |
2020 | Lumasiran | Alnylam | siRNA | HAO1 | Rare genetic liver disease: primary hyperoxaluria type 1 | SC |
2020 | Inclisiran | Novartis | siRNA | PCSK9 | Familial hypercholesterolemia or cardiovascular disease | SC |
2022 | Vutrisiran | Alnylam | siRNA | TTR | Hereditary TTR amyloidosis | SC |
Table 1. Introduction of EMA/FDA approved siRNA drugs
The majority of approved siRNAs and those in late-stage clinical trials feature phosphorothioate (PS) backbone modifications along with multiple 2'-OMe and 2'-F modifications (Table 2). These alterations significantly influence their in vivo and in vitro PK properties.
Drugs | Chemical modifications | Delivery systems | ||
Skeleton | Iminosugar rings | |||
2ʹ-OMe | 2'-F | |||
Patisiran | NA | √ | - | LNP |
Givosiran | PS(6) | √(28) | √(16) | GalNAc |
Lumasiran | PS(6) | √(34) | √(10) | GalNAc |
Inclisiran | PS(6) | √(32) | √(11) | GalNAc |
Vutrisiran | PS(6) | √(35) | √(9) | GalNAc |
Table 2. EMA/FDA Approved siRNA drugs and their structural modificationsa
a. The numbers in parentheses within the table indicate the total count of chemical modifications in each siRNA.
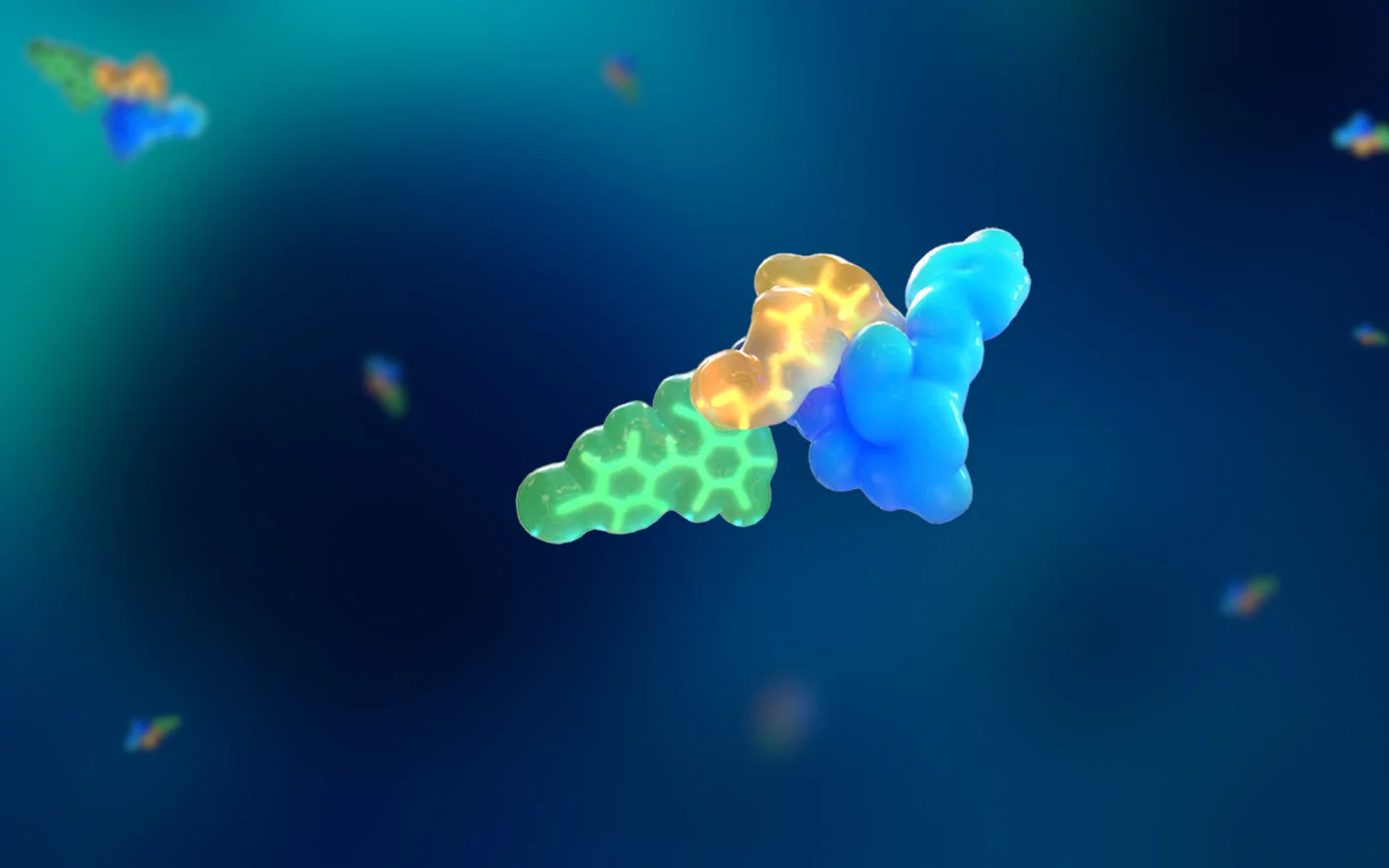
After administration in vivo, siRNA drugs initially enter the blood circulation and subsequently undergo metabolism or excretion in the liver or kidneys (Figure 1). Next, we analyze the PK study data, encompassing ADME and DDI, included in the regulatory approval applications of the aforementioned five siRNA drugs.

Figure 1. In vivo disposition of siRNA after administration1
Absorption of Approved siRNA Drugs
a. How to measure preclinical absorption of the marketed siRNA drugs
Absorption refers to the process by which a drug enters the body from the administration site and is distributed throughout the body via the bloodstream. For Patisiran, male and female Sprague–Dawley (SD) rats and male and female cynomolgus monkeys received intravenous administration at low, medium, and high doses. Plasma concentrations were then analyzed to assess the pharmacokinetic (PK) profiles of the siRNAs and two novel lipid components. As for the four GalNAc-modified siRNAs, namely Givosiran, Lumasiran, Inclisiran, and Vutrisiran, they were administered intravenously at a single dose and repeatedly subcutaneously at multiple doses in male and female SD rats and cynomolgus monkeys. This allowed for the evaluation of the siRNAs' PK profiles after intravenous and subcutaneous administration.
b. Rationale for the route of administration of Patisiran and the other four GalNAc-modified siRNAs
A significant challenge in developing oligonucleotide drugs lies in achieving adequate exposure to target tissues. Unlike most small molecule drugs, oligonucleotide drugs are not readily absorbed in the gastrointestinal tract, necessitating alternative routes of administration such as intravenous (IV) and subcutaneous (SC) routes to achieve sufficient exposure to the target tissues.
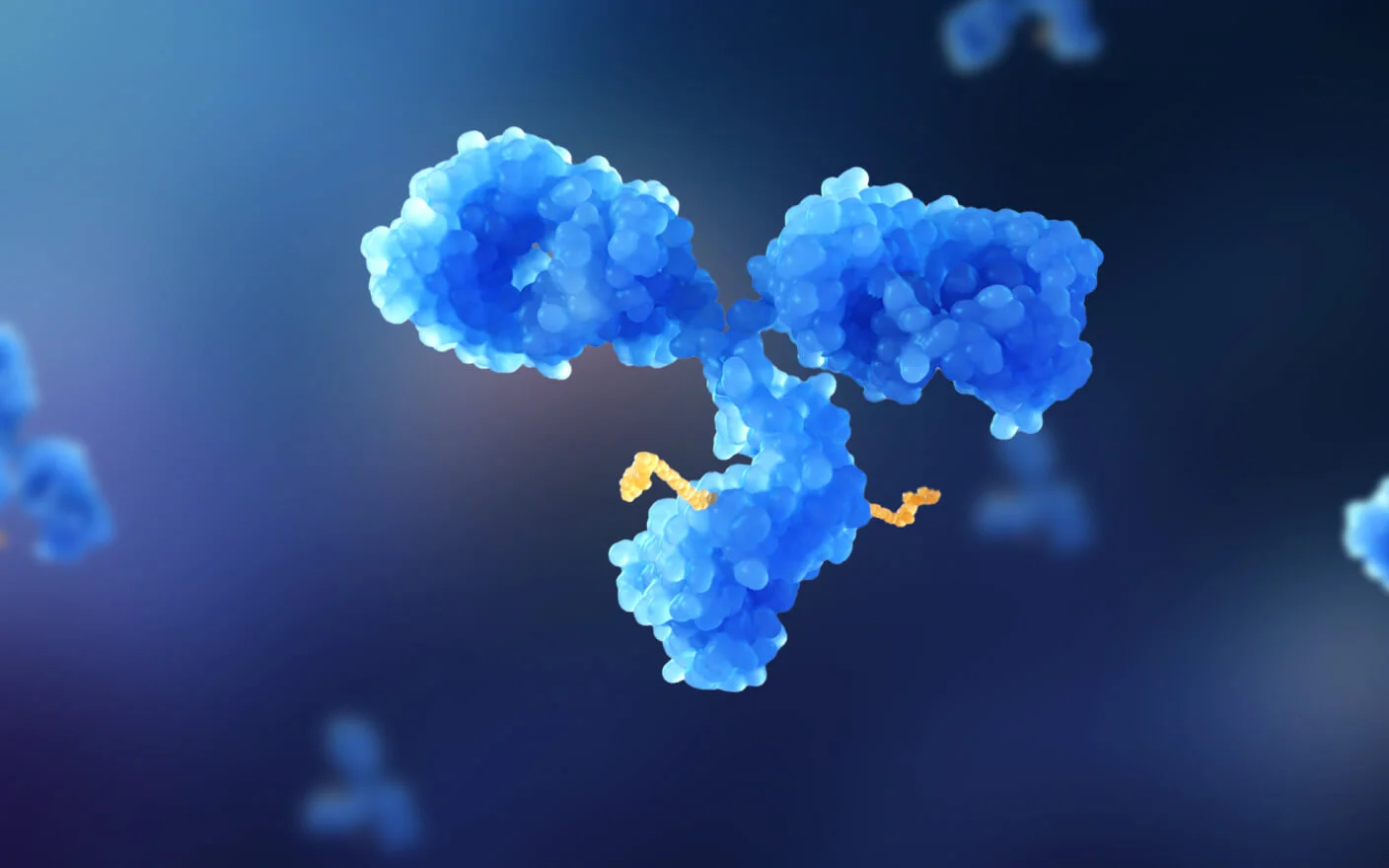
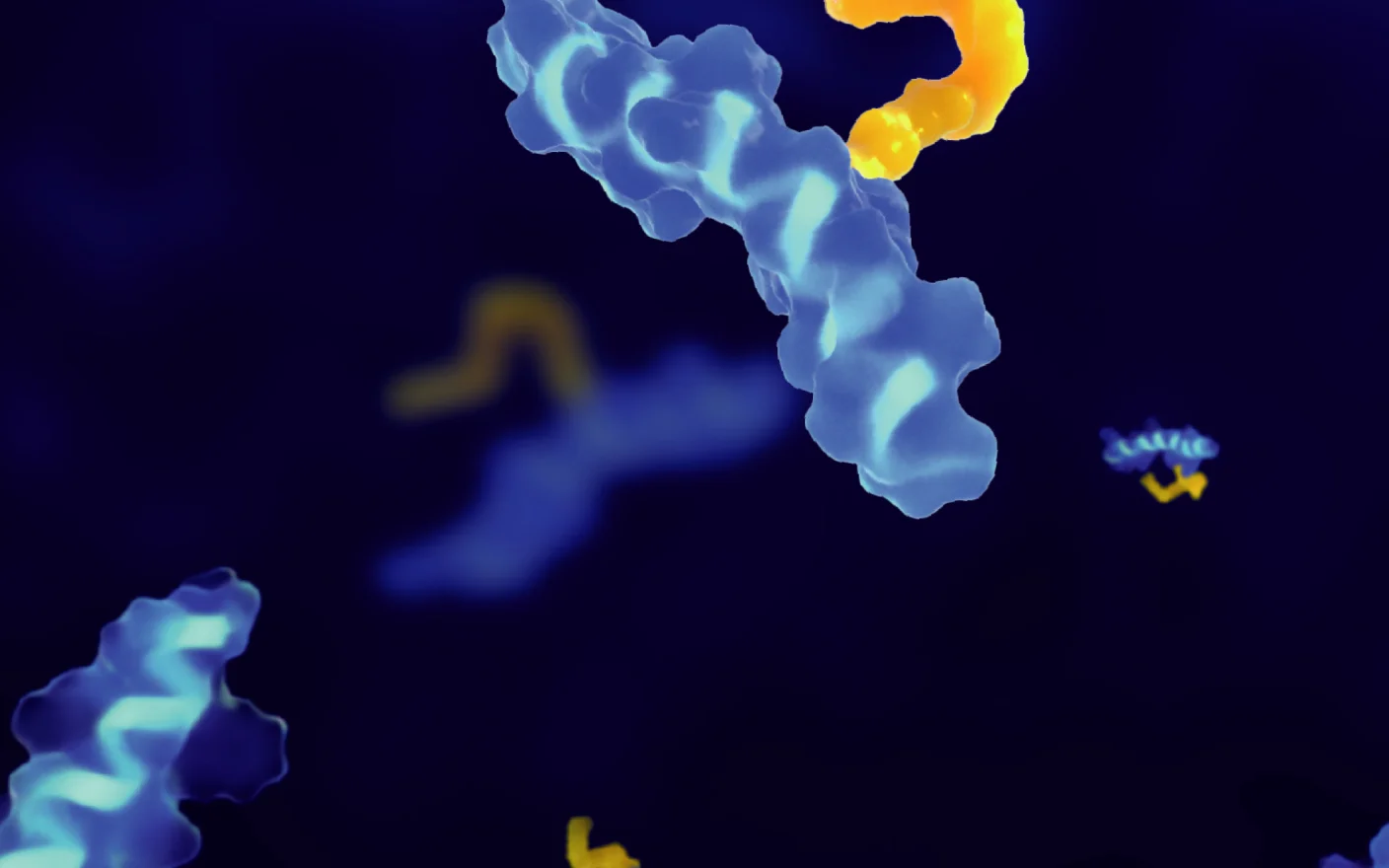
Patisiran, encapsulated in LNPs with a particle diameter of approximately 60–100 nm, achieves notably higher exposure in the liver after IV injection compared to subcutaneous SC injection2. Thus, IV administration was selected for preclinical and clinical testing. Following IV administration, Patisiran is transported to the liver with the aid of plasma apolipoprotein E (APOE), facilitating liver-targeted drug delivery (Figure 2).

Figure 2. Main mechanisms of LNP-siRNA delivery and function3
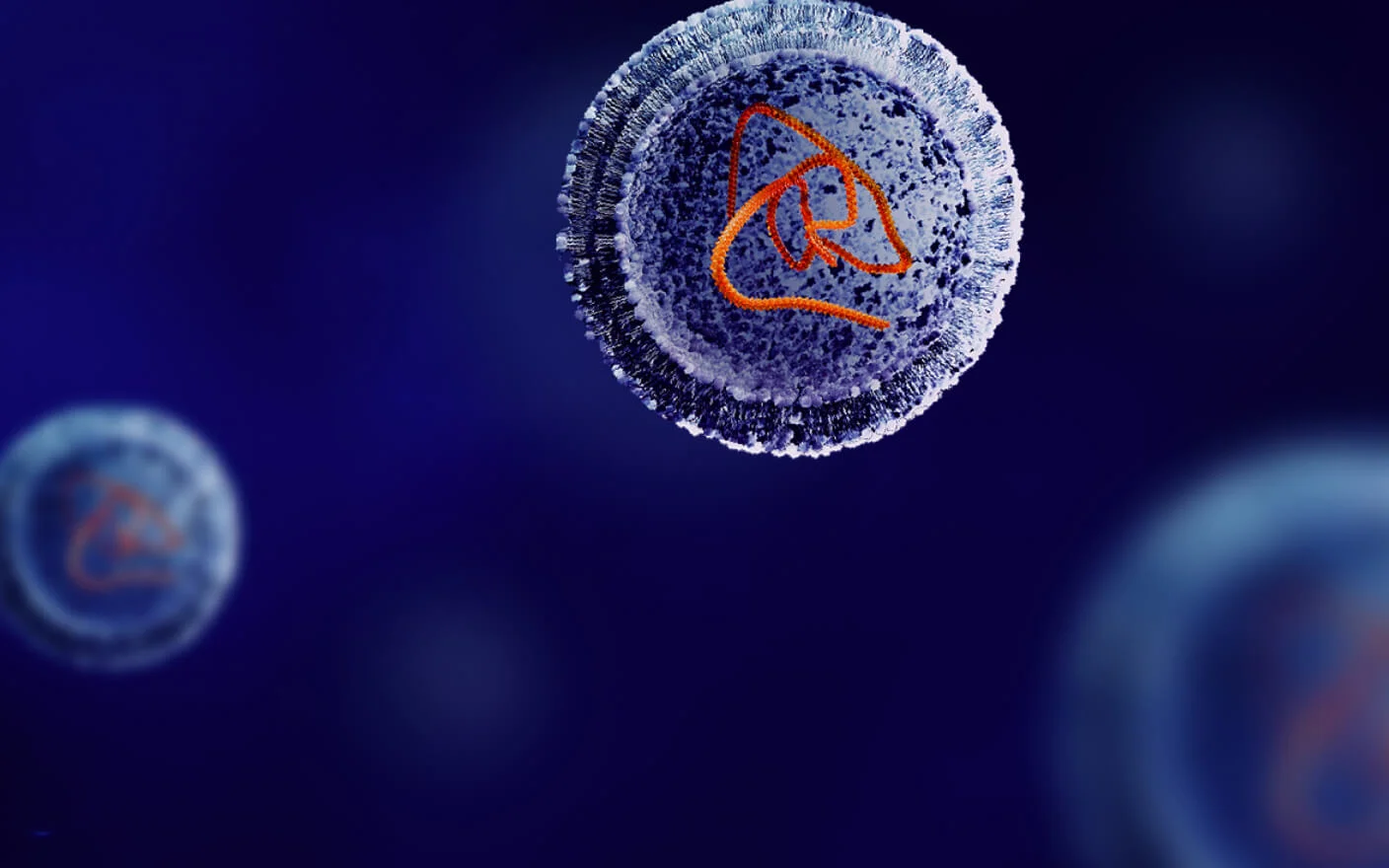
Givosiran, Lumasiran, Inclisiran, and Vutrisiran utilize a delivery system modified with N-Acetyl-D-galactosamine (GalNAc) (Figure 3). These siRNAs are designed to target hepatocytes, taking advantage of the high expression of the Asialoglycoprotein receptor (ASGPR) on the hepatocyte membrane. GalNAc serves as a ligand for ASGPR, facilitating siRNA entry into the target tissue through ASGPR-mediated cellular endocytosis. Hepatocytes have abundant ASGPR, with approximately 500,000 receptors per cell4, leading to saturation effects. Intravenous (IV) administration results in high drug concentrations in the bloodstream, potentially causing ASGPR saturation and reducing the number of drug molecules that can enter hepatocytes. Conversely, subcutaneous (SC) administration offers a sustained-release effect, allowing drug molecules to enter hepatocytes at a slower pace, thereby achieving sufficient exposure to the target tissue.

Figure 3. The major mechanism of liver-targeting by GalNAc-siRNA5
c. Summary and analysis of PK data on the absorption of EMA/FDA approved siRNA drugs
Representative human plasma PK data for Patisiran reveals a characteristic two-compartment model (Figure 4). Following a single IV administration, the blood concentration-time curve shows a rapid decrease in concentration, followed by a secondary peak and linear elimination. The initial decline can be attributed to the drug's rapid distribution in tissues after entering circulation, with a substantial proportion of Patisiran molecules entering the liver from the bloodstream. Subsequently, some Patisiran molecules re-enter the circulation from the liver, resulting in a secondary increase in plasma concentration. The terminal elimination half-life (t1/2) of Patisiran is approximately 2–3 days6, with relatively small apparent distribution volume and plasma clearance rate (Table 3) and a significantly higher area under the concentration-time curve (AUC)in humans than that in rats and monkeys.

Figure 4. PK profiles of approved siRNA drugs after human administration7-11
The PK profiles of Givosiran, Lumasiran, Inclisiran, and Vutrisiran following single-dose IV administration in rats and monkeys were comparable, with t1/2 values of approximately 0.2–0.6 h and relatively small apparent volumes of distribution and plasma clearance (Table 3). Upon single-dose SC administration in rats, monkeys, and humans, these siRNAs exhibited plasma Tmax values ranging from 0.4 to 6 h, with a slightly delayed peak in humans. Moreover, the observed t1/2 ranged from 1 to 9.58 h, showing a longer half-life in humans compared to rats and monkeys. The bioavailability was between 5% to 35.1% in rats and 8% to 25% in monkeys (Table 3). Following SC absorption, the plasma PK profile conformed to a two-compartment model (Table 4). The systemic exposure, measured by plasma Cmax and AUC0-t values, increased roughly proportionally with the dose, and no significant sex differences were observed between male and female animals4–8.
Patisiran | Givosiran | Lumasiran | Inclisiran | Vutrisiran | |||||
IV bolus (R, C) or infusion (H) | IV bolus | SC | IV bolus | SC | IV bolus | SC | IV bolus | SC | |
Dose (mg/kg) | 0.3 | 10 | 5 | 5 (R); 10 (C); | 5 (R); 10 (C); 3 (H) | 5 (R); 6 (C); | 5 (R); 3 (C); 300 mg (H) | 5 (R); 10 (C); | 3 (R); 3 (C); 300 mg (H) |
Tmax (h) | — | — | 0.4 (R); 2.4 (C); 4 (H) | — | 1 (R); 2.4 (C); 3.17 (H) | — | 1 (R); 1.8 (C); 6 (H) | — | 0.5-1 (R); 1.9-2.8 (C); 5 (H) |
Cmax (μg/mL) | 7.07 (R); 3.50 (C); 5.49 (H) | — | 0.43 (R); 0.83 (C); 0.975 (H) | — | 0.581 (R); 2.71 (C); 0.533 (H) | — | 0.787 (R); 0.526 (C); 0.509 (H) | — | 0.492 (R); 0.552 (C); 1.09 (H) |
AUC (μg·h/mL) | 3.40 (R); 6.68 (C); 61.5 (H) | 11.8 (R); 30.5 (C); — (H) | 1.29 (R); 4.65 (C); 7.83 (H) | 7.95 (R); 58.9 (C); — (H) | 1.22 (R); 13.5 (C); 7.21 (H) | 5.36 (R); 26.4 (C); — (H) | 1.88 (R); 3.06 (C); 7.98 (H) | 13.3 (R); 77.6 (C); — (H) | 0.889 (R); 3.26 (C); 15.9 (H) |
%F | — | — | 24 (R) | — | 30 (R), 25 (C) | — | 35.1 (R), 24.7 (C) | — | 5-18 (R), 8-22.3 (C) |
t1/2 | — (R); — (C); 2.18 d (H) | 0.2 h (R); 0.4 h (C); — (H) | 2.7 h (R); 3.5 h (C); 9.29 (H) | 0.4 h (R); 0.6 h (C); — (H) | 1 h (R); 2.6 h (C); 5.98 (H) | 0.3 h (R); 0.6 h (C); — (H) | 1.7 h (R); 2.4 h (C); 9.58 (H) | — (R); — (C); — (H) | — (R); — (C); 5.53(H) |
Vdss (mL/kg) | 27.5 (R); 447 (C); 552 (H) | 181 (R); 104 (C); — (H) | — | 332 (R); 163 (C); — (H) | — | 141 (R); 42.6 (C); — (H) | — | — (R); — (C); — (H) | — |
CL (mL/h/kg) | 88.2 (R); 46.3 (C); 9.35 (H) | 870 (R); 340 (C); — (H) | — | 646 (R); 189 (C); — (H) | — | 950 (R); 229 (C); — (H) | — | 376 (R); 129 (C); — (H) | — |
Table 3. Main PK parameters of EMA/FDA approved siRNA drugs
SC = Subcutaneous, R = Rat, C = Cynomolgus monkey, H = Human;M = Mouse. The abbreviations apply to all subsequent tables.
Distribution of EMA/FDA Approved siRNA Drugs
a. How have these marketed siRNA drugs been evaluated for drug distribution in preclinical studies?
In vitro studies play a crucial role in understanding compound distribution. For example, permeability assays are employed to characterize the ability of a compound to enter cells, while plasma protein binding (PPB) assays quantify the degree of binding to plasma proteins., Higher PPB rates can potentially limit therapeutic efficacy by reducing the concentration of free drugs available to interact with the intended target. Patisiran PPB studies primarily utilized fast protein liquid chromatography followed by sodium dodecyl sulfate–polyacrylamide gel electrophoresis to assess PPB. Other siRNA drug studies employed electrophoretic mobility shift assays to study PPB. These evaluations provide valuable insights into the distribution behavior of siRNA drugs during preclinical investigations.
The in vivo distribution of a drug after administration involves its reversible transfer between different locations within the body. To track changes in drug concentration over time in various tissues and organs, researchers typically employ tissue collection or in vivo ADME studies, such as quantitative whole-body autoradiography (QWBA), utilizing radiolabeled drugs. In the case of these approved siRNA drugs, in vivo evaluations of their distribution have been conducted through major tissue collection after the administration of unlabeled compounds or via QWBA assays, providing valuable insights into their in vivo distribution patterns.
b. Summary and analysis of approved siRNA drug distribution data
In vitro protein binding data reveals that LNP-encapsulated Patisiran displayed a relatively low binding rate to plasma proteins, including albumin and alpha-1-acid glycoprotein. In contrast, the lipid component PEG2000-C-DMG alone exhibited relatively high plasma protein binding (PPB). As for Givosiran, Lumasiran, Inclisiran, and Vutrisiran, they demonstrated an inverse concentration-dependent degree of PPB, where lower concentrations correlated with higher protein binding, and higher concentrations correlated with lower protein binding (Table 4).
Species | Patisiran | Givosiran | Lumasiran | Inclisiran | Vutrisiran |
Human | 97%(PEG2000-C-DMG), 0.46% (serum albumin), 2.07% (alpha-1-acid glycoprotein) | 21-92% (1-50 ug/mL) | 20-85% (0.5-50 ug/mL) | 86-93% (0.5-1 ug/mL) | 19-82% (0.5-50 ug/mL) |
Monkey | — | 26-90% (1-50 ug/mL) | 37-86% (0.5-50 ug/mL) | 86-93% (0.5-1 ug/mL) | 16-87% (0.5-50 ug/mL) |
Rat | 0.89% (serum) | 28-93% (1-50 ug/mL) | 35-96% (0.5-50 ug/mL) | 86-93% (0.5-1 ug/mL) | 26-84% (0.5-50 ug/mL) |
Mouse | — | 10-91% (1-50 ug/mL) | — | 86-93% (0.5-1 ug/mL) | 12-75% (0.5-50 ug/mL) |
Table 4. In vitro PPB of EMA/FDA approved siRNA drugs
The available data on in vivo tissue concentrations of the marketed siRNA drugs consistently demonstrate strong liver targeting, with significantly higher exposure in liver tissues (measured by AUC or Cmax) compared to plasma after administration. Notably, the liver exposure of GalNAc-modified siRNAs is consistently much higher than that of Patisiran (Table 5).
| Patisiran | Givosiran | Lumasiran | Inclisiran | Vutrisiran | ||||
Species | Rat IV | Monkey IV | Rat SC | Rat IV | Rat SC | Monkey SC | Rat SC | Monkey SC | Rat SC |
Dose (mg/kg) | 0.3 |
| 10 | 10 | 1, 5, 10 | 1, 5, 10 | 1, 5, 25 | 1, 3, 6 | 3 |
Liver Tmax (h) | 24 - 72 h (Hepatocyte uptakepatisiran-LNP) | 2 h (Hepatocyte uptake patisiran-LNP) | 1.1 | 2.1 | 4, 6, 8 | 16, 16, 48 | — | — | — |
Liver Cmax (μg/g) | 1.53 | 0.065 | 197 | 102 | 11.1, 65.7, 120 | 31.0, 90.4, 169 | — | — | — |
Liver AUC (μg·h/g) | 5.99 | — | 10494 | 5390 | 1210, 5820, 10700 | 13485, 41600, 76700 | — | — | 3890 |
Liver t1/2 (h) | — | — | 120 | 55 | 191, 105, 138 | 292, 371, 409 | — | — | — |
Plasma Cmax (μg/mL) | 7.07 | 3.5 | 1.07 | 148 | 0.581 (5 mg/kg) | 2.71 (10 mg/kg) | — | — | — |
Plasma AUC (μg·h/mL) | 3.4 | 6.68 | 2.79 | 11.8 | 1.22 (5 mg/kg) | 13.5 (10 mg/kg) | — | — | 33.2 |
Table 5. Target tissue concentration data of marketed siRNA drugs
Radiolabeled quantitative whole-body autoradiography (QWBA) assays reveal that these approved siRNA drugs are predominantly distributed in the liver. Additionally, other blood flow-rich tissues such as kidneys and lymph nodes in immune organs also exhibit higher drug distribution (Table 6).
| Patisiran (14C-DLin-MC3-DMA) | [3H] Givosiran | [14C] Lumasiran | [14C] Inclisiran | [3H] Vutrisiran |
Species | Rat | Rat | Rat | Monkey | Rat |
Dose (mg/kg) | 0.3 | 10 | 10 | 20 | 3 |
Tissue uptake | liver>spleen>kidney> lung>heart>adrenals | liver>kidney cortex>lymph node>kidney | dose site>liver>kidney> adrenal>CNS | liver>kidney> lymph node | liver>lymph node>kidney> thoracic duct |
Table 6. QWBA assay results for radiolabeled marketed siRNA drugs
Metabolism of approved siRNAs
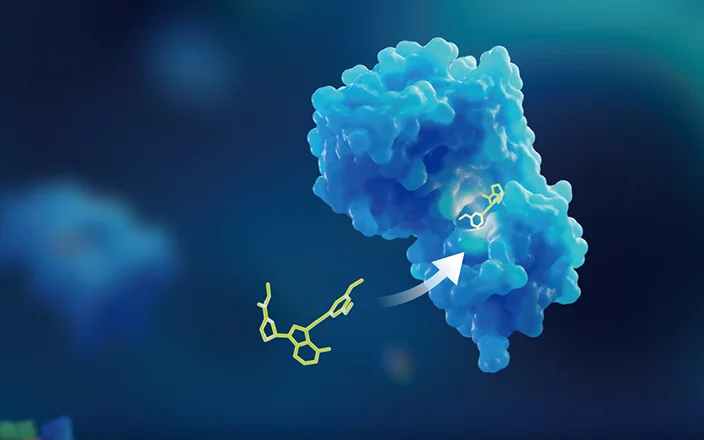
Oligonucleotide is metabolized primarily by endonucleases and exonucleases rather than phase I and II drug-metabolizing enzymes in the liver14. Exonucleases remove one nucleotide at a time from the end of a single strand of siRNA. And endonucleases cleave the strand from the middle of the strand, leaving fragments of different lengths. Following administration, the GalNAc moieties of GalNAc-siRNA are rapidly cleaved by β-N-acetylglucosaminidase during endo/lysosomal trafficking, and the linker is further metabolized by amidase in hepatocytes15. The currently marketed siRNAs are structurally modified and are less likely to be metabolized in system circulation. Typically, the vast majority of siRNAs are rapidly taken up by the liver, with small proportions distributed in other tissues. Then siRNAs are metabolized by nucleases in the liver and other tissues.
a. How the metabolism of approved siRNAs is evaluated in preclinical studies?
The results of in vivo and in vitro metabolism studies of approved siRNAs were summarized in Table 7 and Table 8. For in vitro metabolism studies, liver S9 and serum/plasma stability assays are typically performed. For in vivo metabolism studies, plasma and liver tissues generated during PK studies are usually collected for metabolite profiling. For GalNAc-siRNA, metabolite profiling has been conducted for both the AS and SS, separately. For Patisiran, the LNP-encapsulated siRNA, in vitro and in vivo metabolism of two novel lipid molecules have been additionally examined in addition to the metabolism evaluation of the double-strands.
Liver S9 | Serum | |||
AS | SS | AS | SS | |
Patisiran | 42-77%b | 62-71%(M, R)c,42-44% (C)c, 100% (H)c | ||
Givosiran | 103% (M), 68% (C), 49% (H), 36%(R) | 102% (M), 88% (C), 65% (H), 64%(R) | 75% (M), 59%(R), 63% (C), 89% (H) | 95% (M), 95% (R), 100% (C), 95% (H) |
lumasiran | Stable in many speciesd | 80-85%d | >90%d | |
Inclisiran | >41%d | >64%d | 85% (M), 82%(R), 72% (C), 80% (H) | 95% (M), 91% (R), 91% (C), 87% (H) |
Vutrisiran | 83% (M), 70% (C), 90% (H), 86%(R) | 72% (M), 59% (C), 89% (H), 89%(R) | 95-99%d | 98-101%d |
Table 7. In vitro stability data of EMA/FDA approved siRNAsa
a. Data in the table state the remaining percentage of AS or SS of siRNA after 24-hour incubation in serum or liver S9 matrix.
b. Amount of free siRNA after 6 or 24 h of incubation in serum or S9 matrix.
c. Amount of LNP-encapsulated siRNA after 24 h of incubation in serum.
d. Indicates that the value contains data from rats, mice, monkeys, and human species.
b. Summary and analysis of metabolism data for approved siRNAs
Metabolism data of the marketed siRNAs showed that the in vitro and in vivo metabolic profiles of siRNAs were similar, and these siRNAs shared similar metabolic pathways and metabolites across species including humans (Table 7 and 8). The main metabolic pathway of antisense is the loss of one nucleotide at the 3ʹ end to form the major metabolite, AS(N-1)3ʹ. And that of the sense strand is the loss of one to three GalNAc moieties. Usually, AS(N-1)3ʹ is the main active metabolite. More comprehensive pharmacokinetics evaluation of active metabolites has been performed by researchers in preclinical and clinical studies when the percentage of active metabolites exceeds 10% (e.g. Givosiran).
c. Plasma/serum stability data for AS and SS strands of GalNAc-siRNA
As shown in Tables 7 and 8, the stability of GalNac-siRNA across tested species was similar between serum in vitro and plasma in vivo. And the SS strand was more stable than the AS strand in plasma. This may be due to the presence of the GalNAc group attached to the 3ʹ end of the SS strand, which protects the 3ʹ end of the SS strand from exonuclease-mediated cleavage to a certain extent13. Meanwhile, the presence of the GalNAc motif in the SS strand also protects the 5ʹ end of the AS strand by causing steric hindrance, which may explain why GalNAc-siRNA prefers to form AS(N-1)3ʹ rather than AS(N-1)5ʹ.
| Patisiran | Givosiran | Lumasiran | Inclisiran | Vutrisiran |
Rat/Monkey | 1.Plasma (R): mainly ALN-18238 (siRNA) | 1.Plasma (R, 0–48 h) | Plasma and liver (R, C) | 1.Plasma (R, C) | Plasma and liver (R, C)c |
Human | Plasma: ALN-18328 (less than 5%).d | Plasma: AS(N-1)3ʹ givosirane | Plasma: AS (N-1)3ʹ lumasiranf | Approximately 82.5% of Inclisiran was taken up by the liver | No metabolites were detected in human plasma. |
Major metabolites | Related short strands | AS: AS(N-1)3' givosiran | AS: AS (N-1)3' lumasiran | AS: AS(N-1)3ʹ inclisiran, AS(N-1)5ʹ inclisiran | AS: AS(N-1)3ʹ vutrisiran |
Table 8. In vivo metabolism data of EMA/FDA approved siRNAsa
a. Data in the table were summarized from FDA/EMA information of each marketed drug.
b. In plasma, the ratio of AS (N-1)3ʹ lumasiran was no more than 10%. The 3ʹ deamino metabolite was detected in the monkey liver.
c. Fifteen days after administration, the major drug-related substance in the liver in rats and monkeys was still Vutrisiran.
d. Less than 5% of free double-stranded siRNA was detected in human plasma, indicating that siRNA was still encapsulated by LNP.
e. In human plasma, the concentration of AS(N-1)3ʹ givosiran was approximately half that of Givosiran.
f. The amount of AS (N-1)3ʹ lumasiran was less than 10% of that of Lumasiran in plasma.
Excretion of Approved siRNAs
Oligonucleotide is primarily excreted via the urine due to their polarity, hydrophilicity, and negative charges carried by. During system circulation, the primary elimination pathway of both GalNAc-siRNA and LNP-siRNA is rapid liver uptake followed by slow metabolism in the liver. The secondary elimination pathway is through the kidney.
a. Summary and analysis of excretion data of approved siRNAs
As shown in Tables 9 and 10, the excretion of the five approved siRNAs was evaluated mainly through mass balance studies of radiolabeled and unlabeled test articles. For Patisiran, the excretion evaluation of two novel lipid molecules was conducted. Based on the data from the radiolabeled mass balance study in intact rats (Table 9), the radioactivity recovered in the urine of intact rats ranged from 19.5% to 57.8%, and that in feces ranged from 14.3% to 33.9%. And the radioactivity recovered in bile ranged from 20% to 28.3% in bile duct-cannulated rats. The radioactivity was mainly excreted through urine and bile. The mass balance data in cynomolgus monkeys showed that the radioactivity excreted through urine ranged from 32% to 50% and that through feces ranged from 1.6% to 10%. The results were consistent with that from rats, suggesting that siRNAs were primarily excreted via the urine.
Rat | Monkey | ||||
Urine | Feces | Bile | Urine | Feces | |
Patisiran | 49% | 24% | NA | 50% | 10% |
Givosiran | 30.4%b/57.8% | 1.42%b/14.3% | 27.4 | NA | NA |
Lumasiran | 15.3%b/19.5% | 0.666%b/33.9% | 28.30% | 38% | 8% |
Inclisiran | 29% | 23% | about 20% | 32% | 1.60% |
Vutrisiran | 25.8%b/52.5% | 1.50%b/15.2% | 24.00% | NA | NA |
Table 9. The mass balance data of EMA/FDA approved siRNAs (Hot)a
a. Hot refers to radiolabeled compounds. Data in this table were derived from excretion studies with hot compounds. Data in the table were summarized from FDA/EMA information on each marketed drug. “NA” indicates no relevant data.
b. Mass balance data from bile duct-cannulated rats.
Preclinical data indicated that the metabolic pathway of siRNAs was well-defined and siRNAs had long elimination half-lives in the liver. For safety reasons, no radiolabeled mass balance study has been conducted in human subjects for the approved siRNAs. As shown in Table 10, 14% to 25.8% of intact siRNA was excreted through the urine in humans, most of which was excreted within 24 h after administration, indicating that most of the drug was rapidly uptake by the liver. In rats and monkeys, less than 24% of intact siRNA was excreted via the urine. The clinical data were relatively consistent with the preclinical data. The main elimination route of siRNAs in humans is hepatic uptake and the secondary is renal excretion.
Rat | Monkey | Human | |||||
Urine | Feces | Bile | Urine | Feces | Urine | Feces | |
Patisiran | - | - | - | - | - | <1% | NA |
Givosiran | 10.40% | 0.09% | NA | 15.90% | - | 5-14% | NA |
Lumasiran | <1% | - | NA | 20% | NA | 17.4-25.8% | NA |
Inclisiran | NA | NA | NA | NA | NA | 15.90% | NA |
Vutrisiran | 9% | <1% | NA | 11-24% | 0.01% | 15.4-25.4% | NA |
Table 10. The mass balance data of EMA/FDA approved siRNAs (Cold)a
a. Cold refers to compounds that are not radiolabeled. Data in this table were derived from excretion studies with cold compounds. Data in the table were summarized from FDA/EMA information on each marketed drug. “-” indicates not detected, and “NA” indicates no relevant data.
b. Special considerations for the use of approved siRNAs in individuals with renal impairment
Of the five siRNA drugs on the market, only Inclisiran has been studied in a dedicated clinical PK study in patients with renal impairment. The other four siRNA drugs have only been evaluated for the impact of mild and/or moderate renal impairment on drug concentration and efficacy in population pharmacokinetic (PK) studies16. The results showed that although Cmax and AUC increased in patients with renal impairment, it did not affect the efficacy of siRNA drugs. No dose adjustments were made in patients with mild or moderate renal impairment.
DDI of Approved siRNAs
Although oligonucleotide is not expected to act as substrates of CYP450 enzymes or transporters, theoretically, oligonucleotide could affect the expression of enzymes and transporters by influencing regulatory pathways. For example, some mRNAs, which can be targeted by oligonucleotide, may be involved in transcription and translation processes related to CYP enzyme formation, thus affecting the expression of CYP enzyme.
Table 11 summarized the results and types of DDI assays for each marketed siRNA drug. Except for Givosiran, none of the marketed siRNA drugs exhibited inhibition on CYP enzymes or was substrates or inhibitors of the transporters. The in vitro DDI results of Givosiran showed that Givosiran has some inhibitory effect on P-gp13, but the inhibition is unlikely to occur at clinically relevant dosage. In addition, Givosiran is known to reduce the activity of CYP enzymes viaits pharmacological activity17. For this reason, a dedicated clinical DDI study was conducted on Givosiran.
In general, there is a lack of DDI guidelines related to oligonucleotide drugs, and it is recommended to evaluate the DDI potential as many DDI assays as possible.
Oligo | CYP substrate | CYP inhibitor | CYP inducer | transporter substrate | transporter inhibitor | |
Direct | Time dependent | |||||
Patisiran | Not evaluated | No | Not evaluated | No | No | No |
Givosirna | Not evaluated | No | No | No | P-gp | No |
Lumasiran | No | No | No | Not evaluated | Not evaluated | Not evaluated |
Inclisiran | Not evaluated | No | No | No | No | No |
Vutrisiran | No | No | No | Not evaluated | Not evaluated | Not evaluated |
Table 11. The summary of DDI evaluation for EMA/FDA approved siRNAs*
*: No: no relevant activity; Not evaluated: no relevant assay was performed. Data in the table were summarized from FDA/EMA information on each marketed drug.
Conclusions
This article summarizes the study designs and data analysis from the preclinical PK studies of five approved siRNA drugs, which helps researchers in related fields to better understand the preclinical study of siRNAs. WuXi AppTec DMPK has established a unique pharmacokinetics study methodology and corresponding integrated in vivo and in vitro testing platform on oligonucleotide, which aims to help customers in the development and application of oligonucleotide.
Click here to learn more about the strategies for OLIGO, or talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Authors: Yan Pan, Jiaqi Yuan, Liping Ma, Jing Jin
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,500+ global clients, and have successfully supported 1,200+ IND applications.
Reference
1. Chris MacLauchlin, A. The ADME of siRNA GalNAc conjugates 2020. 16th Oligonucleotide Ther. Soc. (2020).
2. Chen, S. et al. Development of lipid nanoparticle formulations of siRNA for hepatocyte gene silencing following subcutaneous administration. J. Control. Release 196, 106–112 (2014).
3. Mihaila, R. et al. Mathematical Modeling: A Tool for Optimization of Lipid Nanoparticle-Mediated Delivery of siRNA. Mol. Ther. - Nucleic Acids 7, 246–255 (2017).
4. Witzigmann, D. et al. Variable asialoglycoprotein receptor 1 expression in liver disease: Implications for therapeutic intervention. Hepatol. Res. 46, 686–696 (2016).
5. Springer, A. D. & Dowdy, S. F. GalNAc-siRNA Conjugates: Leading the Way for Delivery of RNAi Therapeutics. Nucleic Acid Ther. 28, 109–118 (2018).
6. European Medicines Agency. European Public Assessment Report: Onpattro (patisiran). 44, (2018).
7. Nick Kozauer, MD(Alnylam Pharmaceuticals, I. . Cross-Discipline Team Leader Review. Patisiran NDA (2016).
8. Alnylam. Givosiran NDA MULTI-DISCIPLINE REVIEW.
9. European Medicines Agency (EMA)/Committee for Medicinal Products for Human Use (CHMP). Assessment report for Oxlumo. vol. 31 (2020).
10. Kallend, D., Stoekenbroek, R., He, Y. L., Smith, P. F. & Wijngaard, P. Pharmacokinetics and pharmacodynamics of inclisiran, a small interfering RNA therapy, in patients with hepatic impairment. J. Clin. Lipidol. 16, 208–219 (2022).
11. Habtemariam, B. A. et al. Single-Dose Pharmacokinetics and Pharmacodynamics of Transthyretin Targeting N-acetylgalactosamine–Small Interfering Ribonucleic Acid Conjugate, Vutrisiran, in Healthy Subjects. Clin. Pharmacol. Ther. 109, 372–382 (2021).
12. European Medicines Agency (EMA)/Committee for Medicinal Products for Human Use (CHMP). Assessment Report of Givlaari (givorisan). Assess. Rep. - Givlaari 31, (2020).
13. Li, J. et al. Nonclinical pharmacokinetics and absorption, distribution, metabolism, and excretion of givosiran, the first approved n-acetylgalactosamine-conjugated rna interference therapeutic. Drug Metab. Dispos. 49, 572–580 (2021).
14. Andersson, P. & Den Besten, C. CHAPTER 20: Preclinical and Clinical Drug-metabolism, Pharmacokinetics and Safety of Therapeutic Oligonucleotides. RSC Drug Discov. Ser. 2019-January, 474–531 (2019).
15. McDougall, R. et al. The Nonclinical Disposition and PK/PD Properties of GalNAc-conjugated siRNA Are Highly Predictable and Build Confidence in Translation to Man. Drug Metab. Dispos. DMD-MR-2021-000428 (2021) doi:10.1124/dmd.121.000428.
16. Jing, X., Arya, V., Reynolds, K. S. & Rogers, H. Clinical Pharmacology of RNAi-based Therapeutics: A Summary Based On FDA-Approved Small-interfering RNAs. Drug Metab. Dispos. DMD-MR-2022-001107 (2022) doi:10.1124/dmd.122.001107.
17. Humphreys, S. C. et al. Considerations and recommendations for assessment of plasma protein binding and drug-drug interactions for siRNA therapeutics. Nucleic Acids Res. 50, 6020–6037 (2022)
Related Services and Platforms




Stay Connected
Keep up with the latest news and insights.