Recently, researchers from the University of Connecticut published a review entitled “Absorption, Distribution, Metabolism, and Excretion of US Food and Drug Administration-Approved Antisense Oligonucleotide Drugs.” 1 in Drug Metabolism and Disposition, a leading journal in the field of drug metabolism. They selected ten antisense oligonucleotides (ASOs) (Fomivirsen, Pegaptanib, Mipomersen, Nusinersen, Inotersen, Defibrotide, Eteplirsen, Golodirsen, Viltolarsen, and Casimersen) that have been approved by the US Food and Drug Administration (FDA), summarizing the main absorption, distribution, metabolism, and excretion (ADME) characteristics of ASOs and discussing current knowledge gaps and future research perspectives. In this article, we will interpret some of the highlights from their findings and share our insights.
Introduction to Antisense Oligonucleotide Drugs
ADME are the essential biological processes that determine the pharmacokinetic (PK) parameters, directly impacting the efficacy and adverse drug reactions. Chemical structure, dosage form, administration site, and route of administration are the main determinants affecting ADME characteristics, which in turn affect efficacy and adverse reactions. In recent years, there has been significant progress in the development of antisense oligonucleotides. Antisense oligonucleotides are synthetic single-stranded antisense oligonucleotides with immense potential for disease treatment. They have unique ADME characteristics that are substantially different from those of small-molecule drugs. Understanding their ADME characteristics is fundamental to the development of new ASOs with improved efficacy and safety.
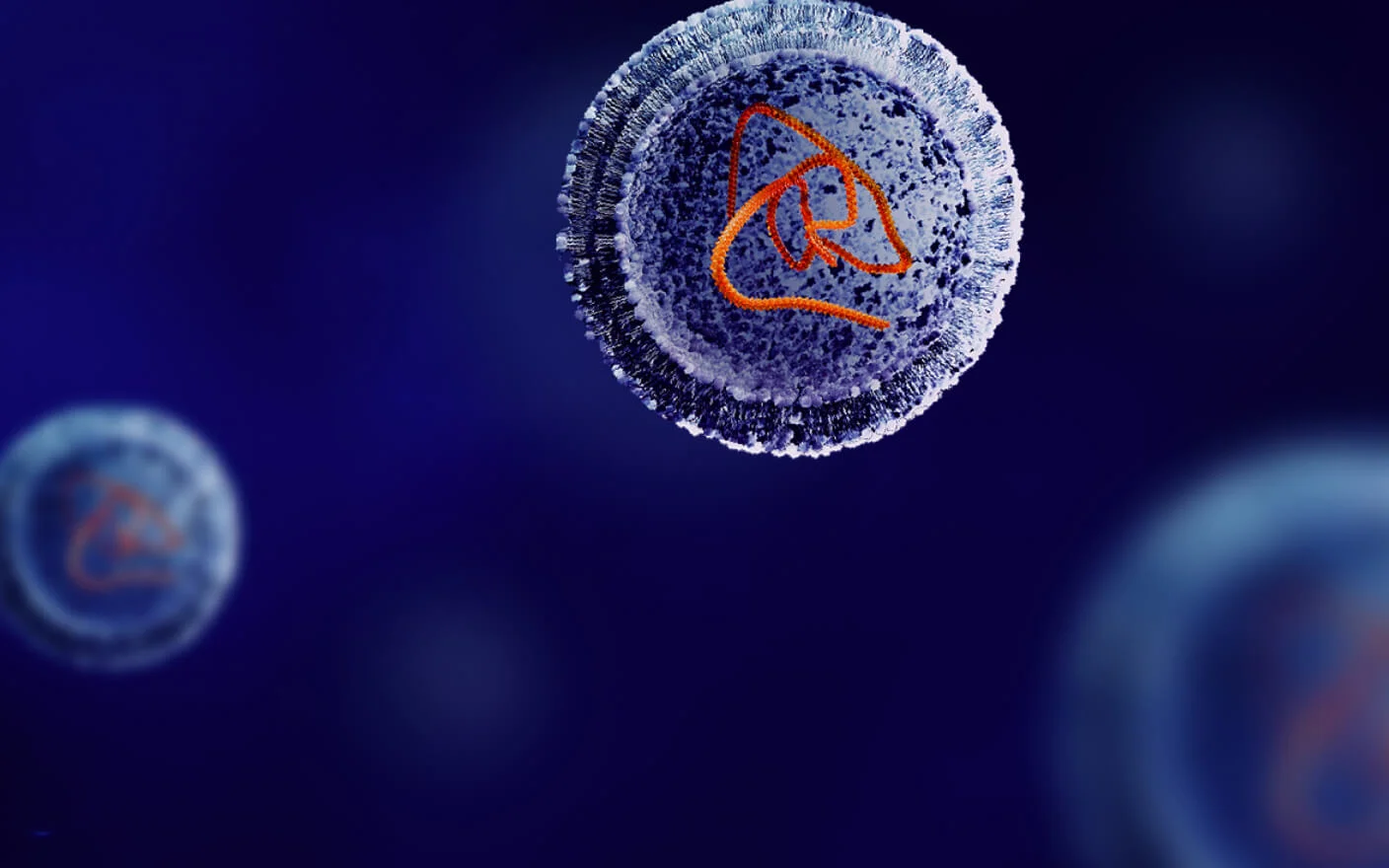
Antisense oligonucleotide drug development can be traced back to 1978 when an oligonucleotide was first discovered to inhibit the translation of Rous sarcoma virus RNA. After nearly 20 years, FDA approved the first ASO drug, Fomivirsen, in 1998 to treat cytomegalovirus (CMV) retinitis (Figure 1). After years of slow approval of new ASOs, the FDA consecutively approved eight ASOs since 2013. In recent years, the ASOs discovery and development platform has been further improved, and more than 100 ASOs are currently enrolled in various phases of clinical trials.

Figure 1. Ten FDA approved antisense oligonucleotide drugs.1
According to mechanisms of action, the ten ASOs approved by the FDA can be divided into five groups.
(A) Inducing RNase H-mediated mRNA degradation: Fomivirsen, Mipomersen, and Inotersen.
(B) Inducing exon skipping: Eteplirsen, Golodirsen, Viltolarsen, and Casimersen.
(C) Nusinersen plays a role in exon restoration.
(D) Pegaptanib is a nucleic acid aptamer, interacting with vascular endothelial growth factor receptors.
(E) Defibrotide is a polydisperse mixture of various single-stranded oligonucleotides, targeting multiple sites to treat veno-occlusive disorder through antagonistic mechanisms.
According to the route of administration, these drugs can be divided into four groups (Table 1).
(A) Intravitreal injection: Fomivirsen and Pegaptanib for the treatment of CMV retinitis in the eye and neovascular macular degeneration in the back of the eye, respectively.
(B) Intrathecal injection: Nusinersen for the treatment of spinal muscular atrophy.
(C) Subcutaneous injection (SC): Mipomersen and Inotersen for the treatment of familial hypercholesterolemia and polyneuropathy of amyloidosis, respectively, administered once weekly.
(D) Intravenous infusion (IV): Defibrotide, Eteplirsen, Golodirsen, Viltolarsen, and Casimersen. Defibrotide is used to treat hepatic veno-occlusive disease by intravenous infusion for 2 h every 6 h. The other four drugs are all used to treat Duchenne muscular dystrophy with weekly infusions.
Route of administration | ASOs | Dosage form | Administration |
(A) Intravitreal injection | Fomivirsen | 0.33 mg drug dissolved in 50 μL solution | Loading dose: administered twice every other week Maintenance dose: every 4 weeks |
Pegaptanib | 0.30 mg drug dissolved in 90 μL solution | Dosing: once every 6 weeks | |
(B) Intrathecal injection | Nusinersen | 12 mg of drug dissolved in 5 mL solution | Loading dose: first three doses with 14 days interval, the 4th dose 30 days after the 3rd dose Maintenance dose: administered every 4 months |
(C) Subcutaneous injection | Mipomersen | 200 mg of drug dissolved in 1 mL solution | Dosing: once a week |
Inotersen | 284 mg of drug dissolved in 1 mL solution | Dosing: once a week | |
(D) Intravenous infusion | Defibrotide | 6.25 mg/kg | Dosing: 2 h of infusion every 6 h for 21 days |
Eteplirsen | 30 mg/kg | Dosing: 35–60 min infusion, once a week | |
Golodirsen | 30 mg/kg | Dosing: 35–60 min infusion, once a week | |
Casimersen | 30 mg/kg | Dosing: 35–60 min infusion, once a week | |
Viltolarsen | 80 mg/kg | Dosing: 60 min infusion, once a week |
Table 1. Administration routes and dosage forms of ASOs1
ADME differs between small molecule drugs and antisense oligonucleotide drugs because ADME of small molecule drugs is mediated by phase I and II drug-metabolizing enzymes, uptake and efflux transporters, transcription factors, and nuclear receptors, whereas ADME of ASO drugs is determined by completely different factors. ASOs enter target cells mainly by endocytosis, which packages them into early endosomes (EE). They then move intracellularly via subcellular trafficking. The metabolism of ASOs is primarily catalyzed by exonucleases and endonucleases, producing shortened-chain oligonucleotides, which are then released into the urinary tract via membrane leakage, in vesicles, or by exocytosis. These characteristics determine the half-life and dosing frequency of ASOs in the circulatory system.
ADME Characteristics of FDA approved Antisense Oligonucleotides
Absorption: The ten approved ASO drugs exhibit multiple absorption patterns that correlate with their indications and administration routes (Table 2).
Fomivirsen and Pegaptanib are used to treat ocular diseases and are administered by local injection into the eye. In rabbits, Fomivirsen is detectable in the retina within hours after injection, with concentrations continuing to increase after 3–5 days. The intravitreal dose is administered at a low dose and is slowly distributed in the eye, resulting in limited systemic exposure. Similarly, Pegaptanib exhibits the highest concentrations in rabbit eyes, where it is slowly absorbed from the eye into systemic circulation and finally excreted via the kidneys. Nusinersen is administered via intrathecal injection, allowing it to bypass the blood-brain barrier to reach the central nervous system. Its concentration in the blood is lower compared to cerebrospinal fluid levels. The other ASO drugs are absorbed systemically, affecting a range of organs throughout the body.
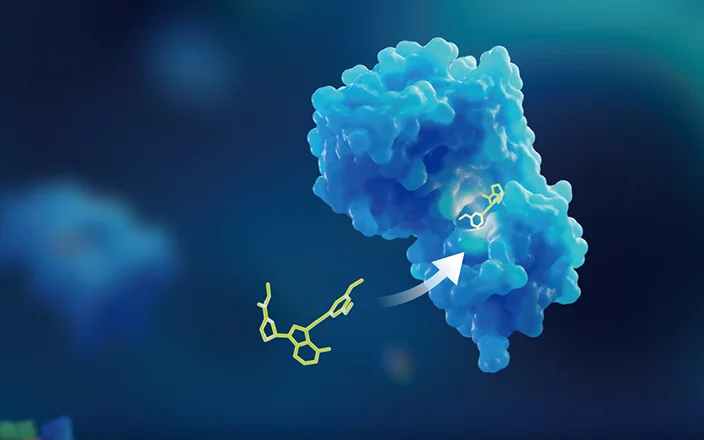
Comments: Unlike small molecule drugs which are mainly absorbed after oral administration, most ASOs require SC or IV administration. After IV administration, ASO drugs are mainly distributed in tissues such as the liver and kidneys, with relatively low distribution in other tissues. Effective delivery of ASOs to specific tissues and organs is a major challenge for future R&D. Various techniques are being explored, including conjugating ASOs with fatty acids, peptides, N-acetylgalactosamine, or cell-penetrating peptides. Some of these strategies have been clinically validated.2
Drug | The site and route of administration | Local/systemic absorption | Blood-brain barrier penetration ability | Tissue with the highest drug concentration | Peak plasma concentration time (h) |
Fomivirsen | Intravitreal injection | Local, Eye | No | Retina, iris; low systemic exposure (below the lower limit of quantification) | Extremely low |
Pegaptanib | Intravitreal injection | Local, Eye | No | Vitreous, retina, aqueous humor, and kidneys | Slow absorption into the systemic circulation |
Nusinersen | Intrathecal injection | Central nervous system, Systemic | Yes | The central nervous system, plasma, peripheral tissues (skeletal muscle, liver, and kidneys), and fat, bone, bone marrow, and spleen | 1.7–6 |
Mipomersen | Subcutaneous injection | Systematic | No | Liver, kidneys, bone marrow, adipose tissue, and lymph nodes | 3–4 |
Inotersen | Subcutaneous injection | Systematic | No | Liver, kidneys, and other tissues | 2–4 |
Defibrotide | Intravenous infusion | Systematic | No | Epithelial cells lining blood vessels in the liver | 2 |
Eteplirsen | Intravenous infusion | Systematic | No | Kidneys and skeletal muscle | 1–2 |
Golodirsen | Intravenous infusion | Systematic | No | Kidneys and all tissues except central the nervous system | 1 |
Viltolarsen | Intravenous infusion | Systematic | No | Kidneys and skeletal muscle | 1 |
Casimersen | Intravenous infusion | Systematic | No | Kidneys and skeletal muscle | 1 |
Table 2. Absorption of ASO drugs 1
Distribution: Plasma protein binding (PPB) affects in vivo drug distribution. The PPB rates and distribution of these ten antisense oligonucleotides vary considerably (Table 3). Inotersen, Nusinersen, Defibrotide, and Mipomersen exhibit high PPB (>90%), while Viltolarsen, Golodirsen, Casimersen, and Eteplirsen display low PPB (<40%). Fomivirsen exhibits lower protein binding values in vitreous samples from rabbit and monkey eyes (<40%). The in vivo steady-state volume of distribution of a drug represents its distribution range in vivo. The steady-state distribution volumes of these ASOs in descending order are as follows: Golodirsen > Eteplirsen > Casimersen, Viltolarsen, Inotersen, and Nusinersen. Notably, the area under the curve (AUC) values for Defibrotide increased by 50%–60% in patients with renal impairment and end-stage renal disease, compared with those patients without renal impairment. There was also a rise in the Peak concentrations by 35%–37% in patients with renal impairment who received dosing.
Comments: Antisense oligonucleotides modified with phosphorothioate (PS) (Fomivirsen, Mipomersen, Nusinersen, and Inotersen) are highly bound to proteins in plasma (especially albumin) due to their negatively charged backbones. The PPB in plasma was not reported in the Fomivirsen application data. Results from our in-house laboratory testing show that PPB is high (>99%) in mouse, rat, monkey, and human plasma at a concentration of 1 μM. ASOs with structures modified by the morpholino subunit (PMO), such as Viltolarsen, Golodirsen, Casimersen, and Eteplirsen, all have neutral backbones and exhibit low PPB. Several PMO-ASOs have common features and high distribution volumes, indicating that they can achieve high distributions in surrounding tissues such as muscles.
Drugs | Biodistribution | |||
Protein binding | Bioavailability | AUC | Distribution volume | |
Fomivirsen | 40% (vitreous samples from treated rabbits and monkeys) | No specific information | No specific information | No specific information |
Pegaptanib | No specific information is available | No specific information | 25 μg/h/mL (3 mg, monocular dose) | No specific information |
Nusinersen | Cerebrospinal fluid: <25% Plasma: >94% | 100% (intrathecal administration) | No specific information | Cerebrospinal fluid: 0.4 L Plasma: 29 L |
Mipomersen | ≥90% clinical therapeutic concentration (1–8 μg/mL) | ~54%–78% | No specific information | No specific information |
Inotersen | >94% (dose-independent) | No specific information | 90 μg/h/mL | 293 L |
Defibrotide | Average of 93% | 100% (IV) | 26.9–48.1 g/mL × h | 8.1–9.1 L |
Eteplirsen | 6%–17% | 100% (IV) | No specific information | 600 mL/kg |
Golodirsen | 33%–39% (dose-independent) | 100% (IV) | 34%–44%* | 668 mL/kg ( at a dose of 30 mg/kg) |
Viltolarsen | ~40% | 100% (IV) | 16%–27%* | 300 mL/kg |
Casimersen | 8%–32% | 100% (IV) | 16%–34%* | 367 mL/kg |
Table 3 Biodistribution of ASOs.1
*Inter-subject variability.
Metabolism: These ten antisense oligonucleotides are metabolized in both blood and target cells. However, they are not metabolized by the liver or by hepatic microsomes in vitro. Therefore, most of the ASOs (Inotersen, Golodirsen, Viltolarsen, Casimersen, Nusinersen, and Eteplirsen) do not interact with conventional drugs and other transporters (Golodirsen, Viltolarsen, and Casimersen). ASOs are primarily metabolized by endonucleases and exonucleases in the blood and in target organs. Most of these drugs are firstly metabolized by endonucleases, which cleave the oligonucleotides into fragments, and then exonucleases can induce hydrolysis reactions at the 3' and 5' ends of the fragments. These drugs are chemically modified to better resist nuclease degradation. Fomivirsen has phosphorothioate bonds in its backbone and belongs to the first generation of therapeutic oligonucleotides. Mipomersen and Inotersen contain 2'-O-methoxyethyl ribose modifications and are regarded as second-generation ASOs with improved resistance to nucleases. Their metabolites have not been found to be pharmacologically active or to pose safety risks to cellular processes.
Comments: Antisense oligonucleotides are not expected to be metabolized by CYP450 enzymes due to their high molecular weights and hydrophilicity. In addition, ASOs enter cells primarily through endocytosis, trapped in endosomes. Intracellular free ASOs are thus less likely to be exposed to CYP enzymes in the endoplasmic reticulum.3,4
Excretion: These antisense oligonucleotide drugs are primarily excreted through the urinary system. Fomivirsen, Eteplirsen, Golodirsen, Viltolarsen, and Casimersen are mainly excreted through the kidneys in unchanged form. Nusinersen, Inotersen, and Mipomersen are mainly excreted as metabolites via the kidneys. These ASO drugs have different half-lives in the body. Some have longer half-lives, including Fomivirsen, which has a half-life of about 55 h in humans and 78 h in monkeys. Nusinersen has a half-life of 135-177 days in cerebrospinal fluid (CSF) and 63-87 days in plasma. The total clearance rate and half-life of Inotersen were 3.18 L/h and 32.3 days, respectively, with a dosage of 284 mg/1.5 mL for one week. Mipomersen has a half-life of 1–2 months. Pegaptanib has a half-life of about ten days in humans after intravitreal injection at ten times the clinical dose. Viltolarsen, Eteplirsen, Golodirsen, and Casimersen have half-lives of 2.5–3.5 h, and Defibrotide has a half-life of several hours. Each of the five ASOs with a short half-life requires intravenous administration.
Comments: Antisense oligonucleotides with higher PPB have reduced glomerular filtration, decreased renal clearance, and thus exhibit longer plasma half-lives. According to the FDA pharmacology review for Mipomersen, its half-life is shorter and clearance is higher in mice compared to humans, which may be associated with the relatively lower PPB in mice.5,6 ASOs with morpholine (PMO) backbones, such as Eteplirsen and Viltolarsen, are very stable to nucleases and do not produce any metabolites after incubation with plasma or hepatic subcellular fractions in vitro, so they are excreted almost entirely in their original form.
Current Knowledge Gaps and Outlook
Based on the regulatory approval application materials for these ten ASO drugs and research data in related fields, the review published by researchers from the University of Connecticut reveals that knowledge gaps exist in the cellular uptake, subcellular trafficking, and cellular efflux of ASOs, and these gaps remain to be filled.
Cellular uptake: It is generally accepted that there are two competing uptake pathways: (1) a “productive uptake pathway” that brings the drug to its target, and (2) a “non-productive pathway” that brings the drug to saturable sinks. To date, key determinants governing the proportions of drugs entering these two pathways are unknown.
Subcellular trafficking and distribution: Small molecule drugs rapidly reach different subcellular regions through uptake by transporters or by diffusion across membranes. ASOs enter cells through endocytic uptake, resulting in their encapsulation in endosomes and subsequent transport to their corresponding targets. Endosomal release and intracellular transport are essential factors in the efficacy of ASOs. Thus, the corresponding mechanisms need to be clarified in the future. It is also important to identify the intracellular locations associated with ASO-mediated cellular damage and ways to prevent ASOs accumulation in these locations.
Cellular efflux: The mechanisms by which the remaining parent and shortened-chain products are excreted from cells after ASOs are broken down by nucleases are unknown. These mechanisms may affect the concentrations of ASOs in plasma and targets.
Comments: ASOs belong to a new class of molecular entities. As such, knowledge gaps exist in scientific knowledge and in regulatory guidance for IND filing. Are current strategies based on small molecule development and application compatible with ASO drugs? Should science-based decisions be further implemented in this industry?
Conclusions
Antisense oligonucleotides have been developed for more than two decades, but there are still numerous unresolved issues and opportunities for innovation in this field. This article provides some insights from the perspective of DMPK to readers. We look forward to more comprehensive industry research on ASO drugs and more development of ASOs.
Click here to learn more about the strategies for OLIGO, or talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Authors: Jie Wang, Xiangling Wang, Genfu Chen
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,500+ global clients, and have successfully supported 1,200+ IND applications.
Reference
[1] Migliorati JM, Liu S, Liu A, Gogate A, Nair S, Bahal R, Rasmussen TP, Manautou JE, Zhong XB. Absorption, Distribution, Metabolism, and Excretion of US Food and Drug Administration-Approved Antisense Oligonucleotide Drugs. Drug Metab Dispos. 2022 Jun;50(6):888-897.
[2] Zanardi TA, Korbmacher B, Boone L, Engelhardt JA, Wang Y, Burel S, Prill B, Aghajan M, Guo S, Henry SP. Safety, Pharmacokinetic, and Pharmacodynamic Evaluation of a 2'-(2-Methoxyethyl)-D-ribose Antisense Oligonucleotide-Triantenarry N-Acetyl-galactosamine Conjugate that Targets the Human Transmembrane Protease Serine 6. J Pharmacol Exp Ther. 2021 Apr;377(1):51-63.
[3] Andersson S, Antonsson M, Elebring M, Jansson-Löfmark R, Weidolf L. Drug metabolism and pharmacokinetic strategies for oligonucleotide- and mRNA-based drug development. Drug Discov Today. 2018 Oct;23(10):1733-1745.
[4] Kazmi F, Yerino P, McCoy C, et al. An assessment of the in vitro inhibition of cytochrome P450 enzymes, UDP-glucuronosyltransferases, and transporters by phosphodiester- or phosphorothioate-linked oligonucleotides. Drug Metab Dispos. 2018 Aug;46(8):1066–1074
[5] Geary RS, Baker BF, Crooke ST. Clinical and preclinical pharmacokinetics and pharmacodynamics of mipomersen (Kynamro®): a second generation antisense oligonucleotide inhibitor of apolipoprotein B. Clin Pharmacokinet. 2015 Feb;54(2):133–146.
[6] Yu RZ, Kim TW, Hong A, Watanabe TA, Gaus HJ, Geary RS. Cross-species pharmacokinetic comparison from mouse to man of a second-generation antisense oligonucleotide, ISIS 301012, targeting human apolipoprotein B-100. Drug Metab Dispos. 2007 Mar;35(3):460-8.
Related Services and Platforms




Stay Connected
Keep up with the latest news and insights.