In recent years, the development of various forms of conjugated drugs has been flourishing, which was strongly led by antibody-drug conjugates (ADCs) with the clinical establishment in cancer therapy. Many other forms of drug conjugates, including peptide-drug conjugates (PDCs) and small molecule drug conjugates (SMDCs), are a focus of current research as well. The mechanism of action of these conjugated drugs is generally similar. The antibody or peptide acts as a precise “navigator” to target the tumor, while the payload acts as the “bullet” with a linker covalently linked in between. After administration, the “navigator” guides the “bullet” to the tumor site followed by releasing the "bullet" to kill the tumor cells, thus exerting specific anti-tumor effects.
While the “navigator” and “bullet” are crucial components of the conjugated drugs, the linker has now been regarded as a critical element as well with the development and the accumulation of clinical experience of drug conjugates. This article introduces the main types of drug conjugate linkers and discusses their effects on the pharmacokinetic (PK), efficacy, and toxicity profiles with representative examples.
Introduction of Linkers of Approved and in Investigational Drug Conjugates
Four types of linkers have emerged in the approved ADCs, including non-cleavable and three cleavable linkers (enzyme-cleavable, acid-cleavable, and GSH-cleavable linkers).1 Specifically, two non-cleavable linkers, three acid-cleavable linkers, eight enzyme-cleavable linkers, and three contain GSH-cleavable linkers appeared in the fourteen approved ADCs (the linkers in Mylotarg and Besponsa are both acid-cleavable and GSH-cleavable, Table 1). Compared to these marketed drugs, the linker is more diversified in the drugs under development. New types of linkers, including Fe (II)-cleavable, photoresponsive cleavable, and biorthogonal cleavable linkers2, have emerged except for the four linkers described above.

Figure 1. Linker Types used in the drug conjugate linkers
|
Drug Name |
Target |
Linkers |
Payload 1 |
Company |
Date of approval |
|
Mylotarg |
CD33 |
Hydrazone and disulfide bonds |
Calicheamicin |
Pfizer |
09/20172 |
|
Adcetris |
CD30 |
MC-VC-PABC |
MMAE |
Seagen |
08/2011 |
|
Kadcyla |
HER2 |
Non-cleavable thioether (MCC) |
DM1 |
Roche |
02/2013 |
|
Besponsa |
CD22 |
Hydrazone and disulfide bonds |
Calicheamicin |
Pfizer |
08/2017 |
|
Lumoxiti3 |
CD22 |
MC-VC-PABC |
Pseudomonas exotoxin A |
AstraZeneca |
09/2018 |
|
Polivy |
CD79β |
MC-VC-PABC |
MMAE |
Roche |
06/2019 |
|
Padcev |
Nectin-4 |
MC-VC-PABC |
MMAE |
Seagen |
12/2019 |
|
Enhertu |
HER2 |
MC-GGFG |
Dxd |
Daiichi–Sankyo |
12/2019 |
|
Trodelvy |
TROP-2 |
Carbonate |
SN38 |
Gliead/Immunomedics |
04/2020 |
|
Vedolizumab |
HER2 |
MC-VC-PABC |
MMAE |
Rongchang Pharmaceuticals |
06/2020 |
|
Blenrep4 |
BCMA |
Non-cleavable MC |
MMAF |
GSK |
08/2020 |
|
Zynlonta |
CD19 |
PEG8-VA-PABC |
Pyrrolobenzodiazepine (PBD) dimer |
ADC Therapeutics |
04/2021 |
|
Tivdak |
TF |
MC-VC-PABC |
MMAE |
Genmab/Seagen |
09/2021 |
|
Elahere |
FRα |
Disulfide bonds |
DM4 |
ImmunoGen Inc. |
11/2022 |
Table 1. Basic information of the 14 Approved ADCs
Note: (1) Structures of some of the payloads are shown in Figure 1 at the end of this article. (2) Mylotarg was initially marketed in 2000, discontinued in 2010, and reapproved to the market in September 2017 by FDA. (3) Due to commercial reasons, Lumoxiti was withdrawn from the European Union in July 2021 and from the United States in July 2023. (4) Blenrep was approved by FDA in 2020 and withdrawn from the market in 2022 due to the failure of Phase III confirmatory clinical trial.

Figure 2. Structures and abbreviations in linker components
Acid-cleavable linkers appearing in the approved ADCs include Mylotarg, Besponsa, and Trodelvy (Figure 3). Acid-cleavable linkers consist of hydrazone and carbonate, which are cleaved mainly in acidic tumor microenvironments (pH 6.5 - 6.9) or in acidic intracellular compartments (i.e., endosomes pH 5.5 - 6.2, and lysosomes pH 4.5 - 5.0), while they remain relatively stable in the blood circulation (pH 7.4). 3 This type of linker achieved the earliest clinical success of Mylotarg. However, the relative instability of acid-cleavable linkers severely limits their application in ADCs because the released payload in the circulatory system may enter non-target cells, increasing the toxic effects of the drug. The first ADC Mylotarg was withdrawn from the market in 2010 due to toxic effects but was subsequently re-approved in 2017 after specifying the patient population and adjusting its administration regimen.

Figure 3. Approved ADCs containing acid-cleavable linkers
Glutathione (GSH) level in plasma is ∼5 μmol/L, while the GSH level in cytoplasm of normal cells reaches 1 - 10 mM. Due to oxidative stress and hypoxia in tumor microenvironments, GSH concentrations can be further elevated in cancer cells which is beneficial to the rapid specific release of payload inside cancer cells 4 when disulfide bond linkers were used. Maytansine derivatives, including DM1, DM3, and DM4 possess intrinsic free thiol groups which can form disulfide bonds with the linker, and they could be directly released after undergoing GSH cleavage (Figure 4a). BCY6135 is such an example which is developed by Bicycle Therapeutics. 1 Most payloads do not have intrinsic free thiol groups and can be conjugated with a self-immolative unit that carries a free thiol group, forming disulfide bonds. (Figure 4b). Examples in this class include mAb-SG3231 and mAb-SG3451. 5
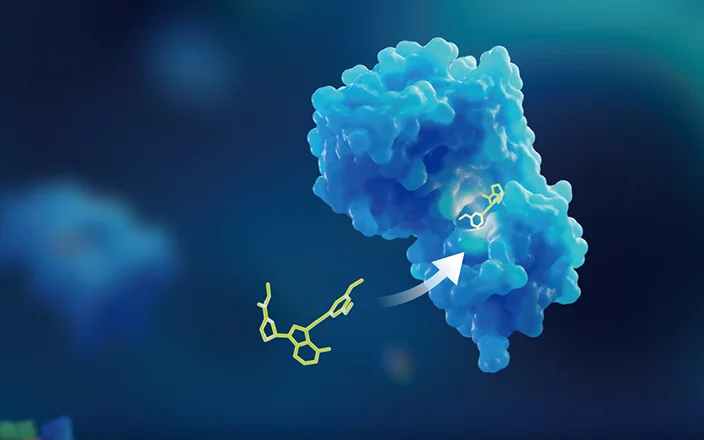
Specific enzymes in intracellular lysosomes or tumor microenvironments can selectively break the linker, for example, proteases in lysosomes hydrolyzing peptide bonds contained in dipeptide or tetrapeptide linkers, glycosidases hydrolyzing β-glucuronides and β-galactosides, phosphatases hydrolyzing phosphoesters and pyrophosphates, and sulfatases hydrolyzing sulfates. 4 The dipeptide linker depicted in Figure 5 requires a hydrophilic residue at the P1 position and a hydrophobic residue at the P2 position so that it could be hydrolyzed by cathepsin. After cleavage of the dipeptide, PABC self-degrades rapidly, leading to the release of the payload.
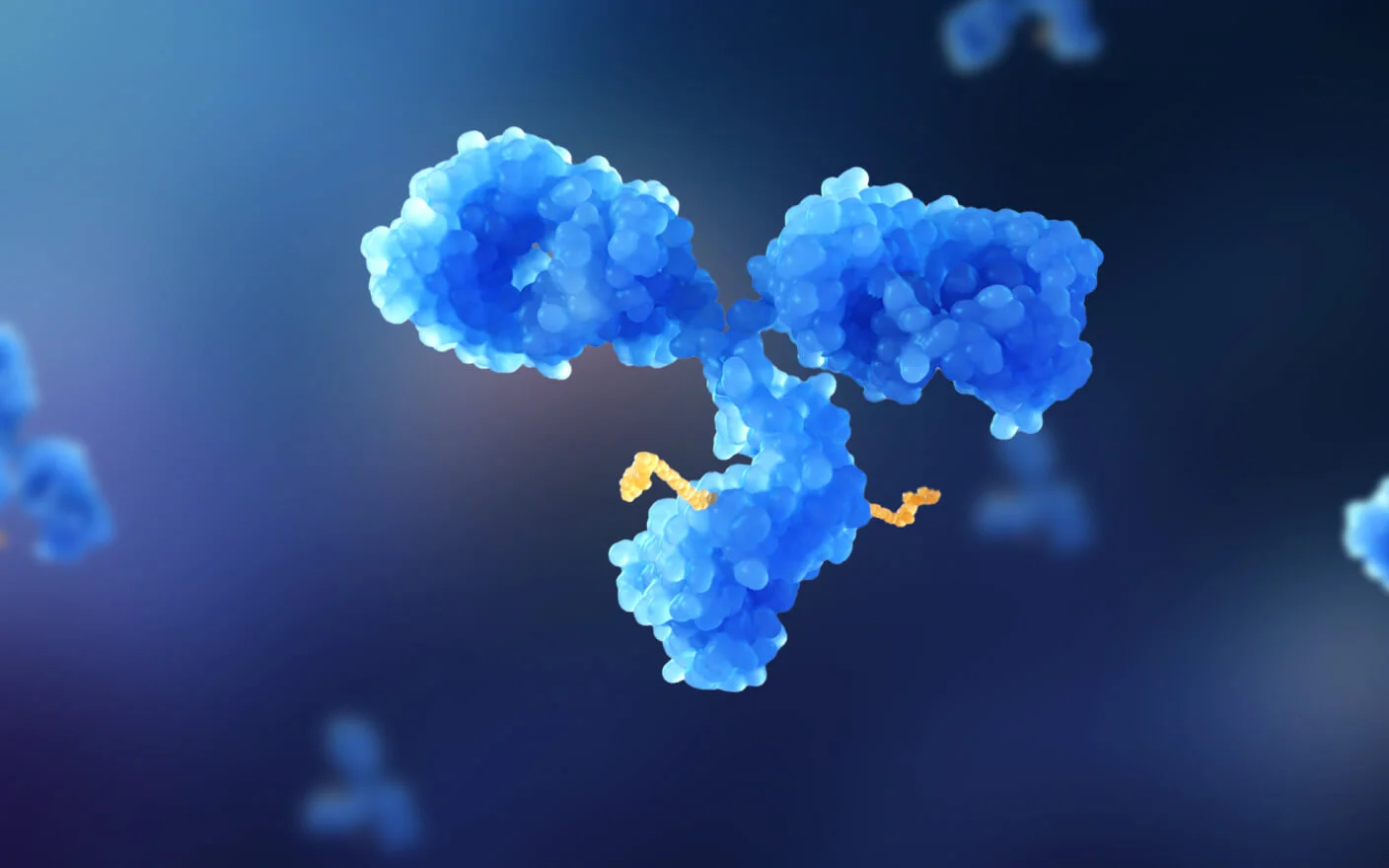
ADCs with non-cleavable linkers need to be internalized and then captured by intracellular lysosomes. Antibodies are hydrolyzed by proteases into peptides or amino acids, which are then progressively broken down into components relevant to the payload to exert efficacy. High expression of targeting antigen on the surface of tumor cells is required for efficient internalization. 6 This type of linker was successfully applied to Kadcyla and Blenrep (Figure 6). The antibody-drug conjugates with non-cleavable linkers usually have longer blood half-life and exhibit reduced off-target effects. Non-cleavable linkers, commonly including maleimide and thiolactam, facilitate the conjugation of payload with antibodies or peptides by forming an amide bond (as in the linker in Kadcyla in Figure 6) or a thioether bond (as in the linker in Blenrep in Figure 6). Oxime and triazole are currently also used in non-cleavable linkers. 1 The properties of these four linkers are summarized in Table 2.

Figure 4. Two types of GSH-cleavable linkers, and the corresponding examples

Figure 5. Example of linker cleaved by cathepsin B

Figure 6. Antibody-drug conjugates containing non-cleavable linkers
|
Acid-cleavable |
GSH-cleavable |
Enzyme-cleavable |
Non-cleavable |
|
- Poor plasma stability and short half-life - Only moderately cytotoxic payloads can be attached |
- Glutathione-induced cleavage - Stable in the circulatory system - Stability is easily influenced by α-substituents |
- More stable than GSH-cleavable and acid-cleavable linkers - Effectively distinguish plasma and target cells - Usually used in combination with self-immolative units such as p-aminobenzyl carbamate (PABC) |
- Requires high antigen expression on tumor cells so that efficient internalization of ADCs occurs - Has a long half-life in the blood, relatively less likely to exhibit off-target effects compared to other types of linkers - Other parts of the conjugated drugs are cracked first, releasing metabolites except for payload before the linker breaks. |
Table 2. Summary of the Properties of the Four Types of Linkers
Considerations for Linker Design of Drug Conjugates
Linker is the unit connecting the payload with a peptide or antibody. In terms of cost and manufacturing difficulty, a linker should be easily connected to the peptide or antibody without affecting the affinity of the peptide or antibody to its receptor. For antibody-drug conjugates, high aqueous solubility is necessary to facilitate biological coupling and prevents inactivation caused by insoluble aggregates.
The development of antibody-drug conjugates has progressed significantly in the last decade resulting from linker improvements and coupling methods. In particular, the linker plays a key role in modulating ADC stability in the systemic circulation and release of the drug for full activity at the target site. 7 Many key parameters of the linker, including branch, electronic charge, polarity, and hydrophilicity affect the PK, efficacy, and toxicity profiles of ADCs (Figure 7).

Figure 7. Considerations for Linker Design of drug conjugates
Drug Conjugate Linker’s Effect on the PK, Efficacy, and Toxicity Profiles
Hydrophilicity is crucial for the development of antibody-drug conjugates, and low hydrophilicity of the linker can cause many problems, such as low coupling efficiency, deposition of ADCs in plasma, and non-specific uptake of ADCs in tissues, and so on. 8 The effects of PEG size on ADC PK and toxicity profile were determined using drug-linkers attached to a nonbinding IgG with a DAR of 8 which were examined in Sprague–Dawley (SD) rats after intravenous administration of 3 mg/kg of the antibody-drug conjugates reported by Burke et al 9. The exposure increased with prolonged PEG length and reached a plateau when the PEG length reached 8. The ADC without PEG chains exhibited rapid non-specific cellular uptake, leading to ADC catabolism and rapid payload release, which reached the peak concentration in plasma and tissue within the first day. The introduction of PEGs containing 4, 8, or 12 PEG resulted in increasingly slower uptake and lower peak concentrations of payload in all tissues (Figure 9A). These antibody-drug conjugates with minimal nonspecific uptake also exhibited less hematological toxicity and reduced histological depletion of bone marrow. After intravenous administration of 20 mg/kg of the ADC without PEG chains, all six SD rats died. Five SD rats died after 10 days of the administration of the ADC containing four monomer PEG chains, and no animals died within 28 days after the administration of the ADC containing 8 or 12 PEG chains. 10 These study results support a strong correlation between ADC hydrophobicity, non-specific uptake rate, payload release, and resulting toxicity. By regulating PEG length, non-specific tissue distribution of ADC in the organism can be ameliorated accordingly, thus effectively reducing off-target toxicity. Methods to improve linker hydrophilicity include the introduction of PEG, sulfonates group, 11 or phosphates group 12 to the linker.

Figure 8. Cleavage mechanism of the ADCs with different PEG lengths

Figure 9. Pharmacokinetics and tolerability of the ADCs in SD rats. A) Plasma pharmacokinetics of the four ADCs after administration of 3 mg/kg of the ADCs to SD rats. B) Survival of SD rats after a dose of 20 mg/kg. In each group of six rats, ADCs with shorter PEG chains resulted in reduced tolerance due to faster non-specific uptake by the tissue 10
Zhang et al. 13 reported their evaluation of the release efficiency of MMAE with different linkers in a BJAB. Luc mouse model targeting CD22 at the same administered dose (20 mg/kg). ADC 3 with a dimethyl-containing linker displayed a higher MMAE release rate (42.1 vs. 19.1 nmol/L) and more potent inhibition of tumor growth (69% vs. 50%) than ADC 1. ADC 2 with PABC linker further enhanced the concentration of MMAE in tumor tissue (87.1 nmol/L) and a 30% tumor regression rate (Figure 10).

Figure 10. Impact of linker structure design on the release efficiency of MMAE
In order to improve ADCs’ efficacy, one method is to avoid or reduce drug resistance of the payload. Antibody-drug conjugates normally employ cytotoxic agents as payloads, but many of them are substrates of the efflux transporter MDR1, which is an important mechanism to generate drug resistance. Most of the reported MDR1 substrates are hydrophobic. Kovtun 14 proposed that if maytansinoids were connected to antibodies via hydrophilic linkers, the resulting metabolites would be hydrophilic. Therefore, they might not be MDR1 substrates, thus avoiding MDR1-mediated drug resistance. To test this idea, they designed ADC 4 and ADC 5 with four PEGs on the linker (Figure 11), which were metabolized by lysosomes into 6 and 7, respectively after internalization into the target cells. The high hydrophilicity of 7 reduces its probability of being an efflux transporter substrate, allowing it to exhibit better therapeutic efficacy. This hypothesis was tested in tumor-bearing mouse models expressing or not expressing MDR1 efflux transporter. ADC 5 showed better efficacy than ADC drug 4 at the same administered dose in mouse models of HCT-15 and COLO 205MDR (both expressing MDR1) tumors, and the efficacy showed a positive correlation with the administered dose. Because of the similar tolerability of the two drugs, ADC 5 showed an improved therapeutic index relative to ADC 4. In a mouse tumor model using COLO 205 cells (which do not express MDR1), no pharmacological difference between ADC 5 and ADC 4 was observed at an equivalent dosage. This example effectively illustrates the reduction of the drug resistance of the payloads by changing the linker could enhance ADCs’ therapeutic index.

Figure 11. Linker design of maytansinoid ADCs and their intracellular metabolism

Figure 12. Efficacy of two antibody-drug conjugates following single subcutaneous injections at three doses of 170, 340, and 680 μg/kg in mouse models of human colon cancer using HCT-15, COLO 205 MDR, and COLO 205 cells.14
The efficacy of antibody-drug conjugates may also be associated with the “bystander effect”. The “bystander effect” involves two mechanisms of action (Figure 13).4 When the antibody-drug conjugates are near the tumor cell, cytotoxic payloads are released within the cell through endocytosis by binding to the antigen on the tumor cell (Figure 13A). In some cases, the payloads may have sufficient membrane permeability to diffuse out of the target cells and kill the surrounding tumor cells. Additionally, instead of internalization, the conjugated drug may release payloads by linker cleavage within the tumor cell microenvironment (Figure 13B), killing not only target cells but also non-targeted cells nearby. The “bystander effect” generally requires cleavable linkers. Non-cleavable linkers usually are not able to exert a “bystander effect” because degraded drugs connecting to amino acids with charges usually lack cell permeability. DS-8201 (Enhertu) achieved great success in treating patients with Her2-low-expressing breast cancer, which is largely attributed to the “bystander effect” that kills nearby tumor cells with no or low HER2 expression. The short plasma half-life of the payload (1.37 h) also attenuates systemic toxicity.

Figure 13. Mechanism of “bystander effect” of conjugated drugs.4
In vitro Linker Cleavage Assays in WuXi AppTec DMPK
Based on different modes of linker cleavage, WuXi AppTec DMPK has established multiple in vitro assays to assess the stability of linkers and to further identify their metabolites (Figure 14). For acid-cleavable linkers, buffers with specific pH values can simulate an acidic environment in the body. For VC-PABC enzyme-cleavable linkers, cathepsin B can trigger intracellular enzymatic cleavage. GSH in a buffer solution can induce the break of the linker for GSH-cleavable linkers. The stability of the non-cleavable linker can be assessed in human lysosomes. In other biological matrices, such as liver S9 fraction or liver homogenate, kidney S9 fraction or kidney homogenate, plasma, and tumor cells, in vitro stability studies or metabolite identification studies can also be performed (Figure 15). The establishment of these assays aims to facilitate the development of effective drug conjugates.

Figure 14. Assays to evaluate payload release with different linkers in WuXi AppTec DMPK

Figure 15. in vitro biological matrices for ADCs’ stability in WuXi AppTec DMPK
Conclusion
With the development and the accumulation of experience of antibody-drug conjugates, linker has been regarded as a crucial element in the ADC design. The traditional four types of linkers have different characteristics, which should be considered in the design of conjugated drugs. Some new linkers with novel mechanisms are also under development, including linkers that utilize exogenous triggers for payload release, which has become a new direction in cleavable linker development. With refinements and progress of the linker, it is believed that more and more drug conjugates will be on the market in the future.

Figure 16. The structures of common payloads
Click here to learn more about the strategies for ADC, or talk to a WuXi AppTec expert today to get the support you need to achieve your drug development goals.
Authors: Qigan Cheng, Xilin He, Jing Jin
Committed to accelerating drug discovery and development, we offer a full range of discovery screening, preclinical development, clinical drug metabolism, and pharmacokinetic (DMPK) platforms and services. With research facilities in the United States (New Jersey) and China (Shanghai, Suzhou, Nanjing, and Nantong), 1,000+ scientists, and over fifteen years of experience in Investigational New Drug (IND) application, our DMPK team at WuXi AppTec are serving 1,500+ global clients, and have successfully supported 1,200+ IND applications.
Reference
[1] Alas, M., et al. Peptide−Drug Conjugates with Different Linkers for Cancer Therapy. J. Med. Chem. 2021, 64, 216.
[2] Su, Z., et al. Antibodye-drug conjugates: Recent advances in linker chemistry. Acta Pharmaceutica Sinica B, 2021, 11, 3889.
[3] Hamann, P. R. et al. Bioconjugate Chem., 2002, 13, 47.
[4] Bargh, J. D., et al. Cleavable linkers in antibody–drug conjugates, Chem. Soc. Rev. 2019, 48, 4361.
[5] Pillow, T. H. et al. Mol. Cancer Ther., 2017, 16, 871.
[6] Ashman, N., et al. Non-internalising antibody–drug conjugates, Chem. Soc. Rev., 2021, 51, 9182.
[7] Su, D., et al. Linker Design Impacts Antibody-Drug Conjugate Pharmacokinetics and Efficacy via Modulating the Stability and Payload Release Efficiency. Front Pharmacol., 2021; 12, 68, 7926.
[8] Lyon R. P., et al. Reducing hydrophobicity of homogeneous antibody‒drug conjugates improves pharmacokinetics and therapeutic index. Nat. Biotechnol. 2015, 33, 733.
[9] Burke, P.J., et al. Optimization of a PEGylated glucuronide-monomethylauristatin E linker for antibody-drug conjugates. Mol. Cancer Ther. 2017, 16, 116.
[10] Simmons, J. K., et al. Reducing the antigen-independent toxicity of antibody-drug conjugates by minimizing their non-specific clearance through PEGylation. Toxicology and applied pharmacology, 2020, 392, 114932.
[11] Zhao,R. Y., et al. Synthesis and Evaluation of Hydrophilic Linkers for AntibodyMaytansinoid Conjugates. J. Med. Chem., 2011, 54, 3606.
[12] Kern, J. C., et al. Discovery of Pyrophosphate Diesters as Tunable, Soluble, and Bioorthogonal Linkers for Site-Specific Antibody−Drug Conjugates. J. Am. Chem. Soc., 2016, 138, 4, 1430.
[13] Zhang, D., et al. Exposure-Efficacy Analysis of Antibody-Drug Conjugates Delivering an Excessive Level of Payload to Tissues, Drug Metabolism and Disposition, 2019, 47, 1146.
[14] Kovtun, Y. V., et al. Antibody-Maytansinoid Conjugates Designed to Bypass Multidrug Resistance. Cancer Res., 2010, 70, 2528.
Related Services and Platforms




Stay Connected
Keep up with the latest news and insights.